Policy/Program Memorandum 169
Date of Issue: June 17, 2024
Effective: September 1, 2024
Subject: Student Mental Health
Application:
Directors of Education
Supervisory Officers and Secretary-Treasurers of School Authorities
Mental Health Leaders
Principals of Secondary Schools
Principals of Elementary Schools
Director of Education, Consortium Centre Jules-Léger
Purpose
The Ministries of Education and Health are committed to working collaboratively to build a continuum of mental health and addictions care across schools, community-based child and youth mental health providers, and hospitals that is coordinated, comprehensive and responsive to the needs of each and every student.
The purpose of this memorandum is to outline requirements for school boards and school authorities, and the Consortium Centre Jules-Léger
The Education Act makes it clear that all partners in the education sector have a role to play in enhancing student achievement and well-being and authorizes the Minister to establish policies and guidelines respecting student mental health, including respecting the use of learning materials relating to student mental health and require boards to comply with the policies and guidelines.
Schools are an ideal place for mental health promotion, the prevention of mental health issues, and the early identification of mental health concerns through school-based intervention services. Schools provide students with the knowledge and skills to be aware of, care for, and advocate for their own mental health and well-being.
Mental health and addictions services and supports should adhere to trauma-informed practices, that are culturally responsive and respect students as individuals with diverse needs and experiences.
Context
Roadmap to Wellness: A Plan to Build Ontario’s Mental Health and Addictions System is the government’s plan to build a comprehensive and connected mental health and addictions system that recognizes the needs of Ontario’s diverse population including children and youth. Implementing the roadmap requires a whole-of-government approach. This policy/program memorandum (PPM) supports the government’s commitment to develop a mental health and addictions system that makes high quality services available for people throughout their lifetime.
Vision Statement for Student Mental Health in Ontario
Students have the knowledge and skills to understand and support their mental health and have access to high quality mental health and addiction services that provide appropriate supports for their diverse needs and experiences when and where they need them across the provincial mental health continuum of care.
Requirements for School Boards
1. Three-Year Mental Health and Addictions Strategy and One-Year Action Plan
Every school board must develop and implement a three-year mental health and addictions strategy and one-year action plan that includes at a minimum, a comprehensive framework that includes the requirements outlined in this PPM and how each component will be evaluated and measured. The board’s mental health and addictions strategy and action plan must be made publicly available on its website by June 30th of the prior school year and reflect input from key partners including students, families and local community-based child and youth mental health providers.
The Ministry will provide a template to school boards on an annual basis to report on the implementation status of the PPM requirements, to be submitted by June 30th, with a copy of the board’s three-year mental health and addictions strategy and one-year action plan.
2. Joint Local Planning with Community-based Child and Youth Mental Health Providers
The work of joint local planning is to support school boards and community-based child and youth mental health lead agencies implementation of a coordinated mental health care system in local communities. This includes:
- Establishing and sharing relevant information between organizations including standardized partnerships, protocols and processes (e.g., Memorandum of Understanding);
- Making the best use of mental health resources in each community by clarifying roles and responsibilities at each tier of service and communicating about the available capacity of local community-based child and youth agencies
- Establishing clear pathways to/through/from mental health care services for students who require services outside of the school setting; and
- Coordinating outreach and engagement with students and their families who may face barriers to accessing mental health care.
To further the vision of “one system of care”
Overall, school boards, Mental Health Leaders, and schools should engage with other interrelated sectors and service delivery partners as needed, as part of system planning efforts (e.g., hospitals, public health units, local Indigenous partners through Indigenous Education Councils and communities, addictions and substance use prevention organizations, cultural and faith-based organizations, organizations addressing gender-based violence, youth advocacy groups).
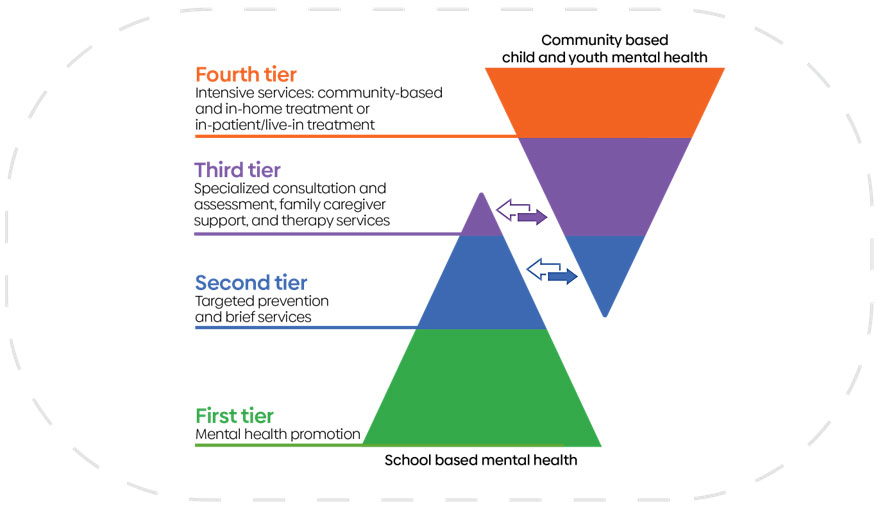
3. Multi-Tiered System of Supports
School boards will utilize a Multi-Tiered System of Supports
4. Consistent Use of Evidence-informed Brief Interventionsfootnote 6 and Standardized Measurement
As appropriate, regulated school mental health professionals will utilize evidence-informed brief interventions and standardized measurement tools that align with their scope of practice and regulatory colleges’ obligations for privacy and reporting. This will allow for opportunities to maximize the best use of resources and meet students’ goals of improved mental health in the school setting. Additionally, the interventions and measurement tools are to be compliant with applicable legislation, such as the Personal Health Information Protection Act, 2004 (PHIPA).
5. Suicide Prevention, Intervention and Postvention Protocols
All school boards will work with their local community mental health and healthcare partners, including Indigenous partners and communities to regularly update and enhance their board’s suicide prevention, intervention and postvention protocols. All school administrators and educators, including guidance teacher-counsellors, must have working knowledge of these protocols and know how to reach out for help immediately on behalf of students.
6. Virtual Care Delivery
When possible, school boards should use an in-person mode of delivery for mental health supports. Remote mental health services using a virtual care platform can be used/offered when it is the most appropriate or accessible delivery vehicle to meet student needs. School boards must use and ensure that the providers of mental health prevention and early intervention services are using a virtual care solution that meets provincial standards for Information & Information Technology solutions to support the safety and security of students and other board users, is compliant with applicable legislation, such as the PHIPA for providing mental health services and aligns with the provider’s scope of practice and regulatory colleges’ obligations for privacy and reporting. It is recommended that virtual care solutions with video and/or secure messaging functionality are verified solutions on the Ontario Health Verified Virtual Visits Solution List, which ensures solutions meet provincial standards for privacy, security and functionality.
7. Enhanced Educator and Staff Mental Health Literacy
School boards will support learning and share evidence-informed resources on mental health and addictions with educators and school staff, including guidance teacher- counsellors, so that they can embed mental health promotion and substance use prevention into the education experience for students and help to foster safe, and welcoming environments.
8. Mandatory Mental Health Literacy Learning for Students
School boards will implement ministry-approved, teacher-led and culturally responsive mental health literacy learning modules for students in Grades 7 and 8 and for students enrolled in the Grade 10 Career Studies course that respect the individual and diverse needs of students and ensure consistency in mental health literacy learning across the province.
The Mental Health Literacy Modules for Grades 7 and 8 are aligned with the existing curriculum expectations in the Grades 7 and 8 Health and Physical Education curriculum. Students will learn about mental health and mental illness and build awareness of the impact of stigma associated with mental illness. In preparation for the transitions that come with adolescence, students will continue building strategies for supporting their mental health, including self-care strategies to maintain good mental health and to know where and when to seek help.
The Mental Health Literacy Modules for Career Studies (GLC2O) are aligned with the revised mental health literacy expectations in the Grade 10 Career Studies course, 2024 (GLC2O), a compulsory course for achieving the Ontario Secondary School Diploma. The modules will support students to learn more about how to use strategies to help manage stress, recognize signs that could indicate stress is becoming problematic, and how to find and access support when needed.
For students with special education needs, the Individual Education Plan (IEP) is the written plan describing the special education program and/or services required by a particular student, based on a thorough assessment of the strengths and needs that affect the student’s ability to learn and to demonstrate learning. Appropriate accommodations and modifications recorded in a student’s IEP must be implemented by the teacher when each module is taught.
9. Family Mental Health Literacy and Awareness
Parents and families play a critical role in supporting the mental health of students and should be involved in their children’s mental health journey when possible. In support of meaningful engagement with families, school boards will make available culturally responsive family mental health literacy resources to ensure that families have access to high quality information about how best to notice and respond when their child may be struggling with their mental health, reduce the stigma that surrounds mental health and mental illness, and provide appropriate supports for their child’s individual needs. This includes educational and engagement opportunities for families through school community outreach efforts.
10. Social-Emotional Learning
Social-emotional learning skills help students foster overall health and well-being, good mental health, and support the ability to learn and thrive. The social-emotional learning skills that are embedded in the Ontario curriculum include: identification and management of emotions, recognizing sources of stress and coping with challenges, maintaining positive motivation and perseverance, building healthy relationships, developing self-awareness and confidence, and thinking critically and creatively.
As emerging research shows the impact that the evaluation of social-emotional learning skills can have on particular groups of students (e.g., Black, Indigenous, racialized students, male students, students with disabilities and students experiencing other socio-demographic disadvantages), educators are not to assess, evaluate or report on the overall expectations related to social-emotional learning skills in the Ontario curriculum. It is the ministry’s expectation that instruction of the social-emotional learning skills will continue.
11. Mental Health Absences
Emphasizing the importance of self-care and prioritizing mental health can allow for more open conversations amongst students, parents, and teachers. If students are unable to attend school due to a mental health concern, their absence must be excused under s. 21(2)(b) (“by reason of sickness or other unavoidable cause”) of the Education Act. Should the student/parent be unable to provide appropriate supporting documentation for the absence, a principal may still excuse the student from attendance at school temporarily under subsection 23(3) of Regulation 298: OPERATION OF SCHOOLS - GENERAL under the Education Act, at the written request of a parent or the pupil where the pupil is an adult.
Principals and school board staff responsible for student attendance may wish to work closely with their school board Mental Health Leader and should consult the Ministry of Education’s Enrolment Register Instructions for Elementary and Secondary Schools for further guidance.
Implementation
School Mental Health Ontario (SMH-ON) is the Ministry of Education’s implementation partner for student mental health. SMH-ON does this through the development and implementation of made-in-Ontario, evidence-informed mental health promotion and prevention resources, programs, and professional learning for classroom educators, school administrators, and regulated school mental health professionals. School boards are expected to work closely with SMH-ON to support the provision of evidence-informed approaches to school-based mental health promotion, prevention and early intervention.
Similarly, the Knowledge Institute on Child and Youth Mental Health and Addictions, partners with the Ministry of Health, the community-based child and youth mental health sector and SMH-ON to share knowledge, build capacity, and create connections to help improve mental health and addictions services for children and youth and their families.
Both organizations are key partners in supporting the implementation of quality mental health services for students and their families across the care continuum.
The implementation of this memorandum should consider the intersections of student mental health with other ministry PPMs including but not limited to:
- Policy/Program Memorandum 81: Provision of health support services in school settings;
- Policy/Program Memorandum 119: Developing and implementing equity and inclusive education policies in Ontario schools;
- Policy/Program Memorandum 128: The Provincial Code of Conduct and School Board Codes of Conduct;
- Policy/Program Memorandum 144: Bullying prevention and intervention;
- Policy/Program Memorandum 149: Protocol for partnerships with external agencies for provision of services by regulated health professionals, regulated social service professionals, and paraprofessionals;
- Mandatory professional activity days devoted to provincial education priorities
The Ministry of Education expects all decisions that support student mental health and well-being to be made in accordance with this PPM and applicable laws, including the Ontario Human Rights Code, and with school board collective agreements. Where any direction of the PPM conflicts with these requirements, the applicable laws and collective agreement provisions prevail.
Roles and Responsibilities
The Ministry of Education recognizes that each school board has a unique complement of professionals that are employed by their board. The roles of school board professionals and the responsibilities outlined in this section are intended to be examples and is not an exhaustive list. School boards are required to abide by collective agreements, each professionals’ scope of practice and requirements of their regulatory college, and applicable legislation.
Ministry of Education
The Ministry of Education provides guidance, funding, and implementation support to school boards to help promote student mental health. The ministry also works with other partner ministries such as the Ministry of Health to support a more systematic approach to children’s mental health and to make the best possible use of resources across the continuum of mental health care.
Ministry of Health
The Ministry of Health has the provincial policy mandate for the overall mental health and addictions system. In March 2020, the ministry released Roadmap to Wellness, Ontario’s mental health and addictions strategy. The Mental Health and Addictions Centre of Excellence at Ontario Health is responsible for implementing Roadmap to Wellness with guidance and funding from the Ministry of Health. The ministry also provides strategic program management and fiscal oversight of community-based child and youth mental health programs and services under the authority of the Child, Youth and Family Services Act, 2017. The Ministry of Health collaborates with the Ministry of Education to support a more integrated system of mental health care for students.
School Boards
School boards are responsible for a number of activities including but not limited to administering the funding they receive from the province for their schools, hiring teachers and other staff including mental health professionals, supervising the operation of schools and their teaching programs, and ensuring schools operate in accordance with the Education Act and its regulations.
Community-based Child and Youth Mental Health Agencies
Community-based child and youth mental health agencies deliver a range of mental health services to children and youth up to the age of 18, and their families. Services are primarily based on a set of provincially defined child and youth mental health “core services,” ranging from prevention services, counselling, and therapy to intensive and specialized services.
Children and Youth Mental Health (CYMH) Lead Agencies
CYMH Lead Agencies are child and youth community-based mental health agencies which are also accountable for planning the delivery of core services in their area and which work with the health, education, and child welfare sectors, including hospitals, schools, and Children’s Aid Societies, to better coordinate services and supports for young people. The CYMH Lead Agency Consortium is a group that represents all 31 Lead Agencies and provides them the opportunity to collaborate, address common challenges, and share information on promising practices, as well as provide coordinated advice to the Ministry of Health.
Public Health Units
Ontario’s 34 Public Health Units offer healthy living programs and disease prevention information for individuals across the lifespan. As a requirement under The Ontario Public Health Standards: Requirements for Programs, Services, and Accountability (Standards), boards of health are required to consider mental health promotion under four different program standards: Chronic Disease Prevention and Well-Being, Healthy Growth and Development, School Health, and Substance Use and Injury Prevention. Under the Mental Health Promotion Guideline, 2018, and School Health Guideline, 2018, boards of health shall develop and implement a program of public health interventions using a comprehensive health promotion approach to improve the health of school-aged children and youth.
Superintendent with Responsibility for Mental Health
The Superintendent with Responsibility for Mental Health provides overall strategic direction in the area of student mental health and ensures this work is communicated and aligned throughout the school board. System and school leaders establish the conditions for quality, consistency and sustainability in school mental health.
Mental Health Leaders
Every school board employs a Mental Health Leader to provide leadership within their school board for student mental health. Mental Health Leaders collaborate with school board staff and community mental health partners to promote a proactive, integrated system of care, with clear pathways to/from/through service for students requiring mental health supports.
Mental Health Leaders are experienced, regulated mental health clinicians who are accountable for developing and implementing their school board’s three-year mental health and addictions strategy, one-year action plan, and the collection, utilization and reporting of information related to student mental health.
Regulated School Mental Health Professionals
Regulated school mental health professionals, including social workers, psychologists, and psychotherapists support students with mild to moderate mental health concerns and provide brief evidence-informed early interventions. For students with more intensive mental health concerns, regulated school mental health professionals will refer students to community-based child and youth mental health services. However, regulated school mental health professionals will support students with intensive mental health concerns and/or students in crisis, as appropriate, when intensive mental health services are not readily available in the community.
Non-regulated School Mental Health Professionals (Student Support Staff)
Non-regulated school mental health professionals, (e.g., child and youth workers) support all students in the classroom or in small groups with evidence-informed mental health literacy and universal mental health promotion activities.
Mental Health and Addictions Nurses in Schools
Mental Health and Addictions Nurses in Schools are employees of Home and Community Care Support Services who provide early intervention, system navigation, and therapeutic strategies that address specific mental health and addiction needs for students. The program consists of specialized nurses working in the community and in schools to assist students who have various mental health challenges.
Educators
Educators are well-positioned to teach all students about mental health. Mental health and well-being is included in the Program Planning section for all Ontario curriculum. In addition, there are mental health related expectations included in various elementary and secondary Curricula. Educators are at the center of creating mentally healthy, and welcoming classroom environments and notice students about whom they may have a concern and know how to respond to those observations. Educators are aware of the pathways to support available in their school when they do notice a student about whom they are concerned.
Guidance Teacher-Counsellors
Guidance teacher-counsellors support career counselling as well as student well-being and make connections to supports for student mental health.
Data Collection, Monitoring and Evaluation
The collection and use of data and evidence to monitor and evaluate student mental health and addictions needs and progress will identify where gaps may exist. All collection, storage, and dissemination of student data and information must be in compliance with obligations under the Municipal Freedom of Information and Protection of Privacy Act (MFIPPA) and PHIPA, as applicable
Data and evidence will inform both the Ministry of Education and school boards that the supporting conditions for student mental health and well-being in schools have been established.
School boards are required to annually report to the Ministry of Education on their activities to achieve the requirements outlined in this memorandum and to use data to inform their three-year mental health and addictions strategy and one-year action plan. The EDU Annual School Mental Health Survey will be comprised of questions that capture information about mental health supports and services provided by school boards, mental health literacy instruction for students, and collaboration with community-based child and youth mental health providers.
Review Process
To ensure information and practices related to student mental health and addictions are current and evidence-informed, this PPM will be reviewed every five years.
Appendix A: Glossary of Terms
- Mental health
- is the state of an individual’s psychological and emotional well-being. It is a necessary resource for living a healthy life and a main factor in overall health. It does not mean the same thing as mental illness. However, poor mental health can lead to mental and physical illness. Good mental health allows you to feel, think and act in ways that help you enjoy life and cope with its challenges.
footnote 7 - Mental illness
- is defined as alterations in thinking, mood or behaviour associated with significant distress and impaired functioning in one or more areas such as school, work, social or family interactions or the ability to live independently.
footnote 8 - Addiction
- is a complex process where problematic patterns of substance use or behaviours can interfere with a person’s life. Addiction can be broadly defined as a condition that leads to a compulsive engagement with a stimuli, despite negative consequences. This can lead to physical and/or psychological dependence. Addictions can be either substance related (such as the problematic use of alcohol or drugs) or process-related, also known as behavioural addictions (such as gambling or internet addiction). Both can disrupt an individual’s ability to maintain a healthy life.
footnote 9 - Substance Use and Mental Health
- When mental health issues and substance abuse occur together, they are called concurrent disorders. Mental health issues and substance abuse problems occur on a continuum, and a concurrent disorder emerges when they intersect at any point. For example, a person might use alcohol to cope with feelings of anxiety or use drugs to cope with symptoms of Attention Deficit Hyperactivity Disorder.
footnote 10 - Mental Health Promotion: Providing universal supports for all students (Tier 1) -
- This is the foundational everyday work that educators and school staff do within and beyond the curriculum to welcome and include students, to understand them, to build knowledge of mental health, to promote mentally healthy habits and to partner with families, students and other staff to create a supportive environment. Most of the mental health work in schools is at this level.
footnote 11 - Prevention and Early Intervention: Targeted evidence-informed help for students requiring additional support (Tier 2) -
- In school, there will be some students who may need additional support.. Educators and school staff can help by reinforcing skills and working to remove barriers to learning. Regulated school mental health professionals and others with specialized skills provide intervention services, like school-based brief interventions.
footnote 12 - Intervention and Pathways to Care: Bridging and crisis management support for students who require more intensive treatment and access to services from community partners (Tier 3) -
- Although it will always be necessary for regulated school mental health professionals to provide some level of intensive services (because students cannot or will not access outside supports, and to manage crisis events as they arise), it is the role of school mental health professionals to help students access appropriate community or health services and to provide needed ongoing care while students are at school.
footnote 13 - Intensive services for community-based and/or in-home treatment or in-patient/live-in treatment (Tier 4) -
- These services are provided by community-based mental health agencies or hospitals for students with the most intense and complex mental health challenges. The role of regulated school mental health professionals is to support student referrals to Tier 4 services, support case management/coordinate with other services the student may require, and support students’ reintegration back to the school environment.
footnote 14 - School-based Brief Interventions
- is an approach to mental health services, delivered in schools that is systematic, brief and evidence-informed for students experiencing mild to moderate mental health concerns. It can be provided to individuals or in small groups.
footnote 15 - Measurement-based Care
- is the routine, systematic use of validated measures, such as patient-reported symptom-rating scales, before or during each clinical encounter to inform decision-making about treatment.
footnote 16 - Trauma-Informed Practice
- recognizes the signs and symptoms of trauma, realizes the extensive impact of traumatic stress on individuals and communities, responds by integrating knowledge of trauma into the program or service, and actively resists the re-traumatization of clients and staff.
footnote 17 - Culturally Responsive
- is an approach to mental health learning, supports and services that considers students’ intersecting social and cultural identities. This approach recognizes that students may respond differently to mental health learning, supports and services and that these differences may be connected to a student’s background, language, family structure, and social or cultural identities. This approach also emphasizes that educators and school leaders reflect on their own biases and analyze how their own identities and experiences affect how they view, understand, and interact with all students.
footnote 18
Footnotes
- footnote[1] Back to paragraph In this memorandum, references to parent(s) and families are aligned with definitions of parent(s) and guardian(s) as used in the Education Act. It may also be taken to include caregivers or close family members who are responsible for raising the child.
- footnote[2] Back to paragraph Wherever school boards are referenced, school authorities and the Consortium Centre Jules-Léger are also included.
- footnote[3] Back to paragraph This policy is established under the authority of paragraph 29.6 of s. 8(1) of the Education Act which authorizes the Minister to establish policies and guidelines respecting student mental health and require boards to comply with the policies and guidelines.
- footnote[4] Back to paragraph School and Community System of Care Collaborative. (2022). Right time, right care: Strengthening Ontario’s mental health and addictions system of care for children and young people.
- footnote[5] Back to paragraph Stephan, S. H., Sugai, G., Lever, N., Connors, E. (2015). Strategies for integrating mental health into schools via a multitiered system of support. Child and Adolescent Psychiatric Clinics of North America, 24(2), 211-231.
- footnote[6] Back to paragraph Brief services (e.g.4-6 sessions) provide “quick access” to therapeutic encounters to address the immediate or presenting needs of a student. Therapeutic approaches include but are not limited to solution-focused, cognitive-behavioural, motivational interviewing and brief narrative therapies. Brief services may meet the needs of the child or young person and be all the treatment that is required or it can help identify or clarify the need for further treatment or services
- footnote[7] Back to paragraph Public Health Agency of Canada
- footnote[8] Back to paragraph Public Health Agency of Canada
- footnote[9] Back to paragraph Canadian Mental Health Association
- footnote[10] Back to paragraph Canadian Centre on Substance Abuse. When Mental Health and Substance Abuse Problems Collide: Understanding, Preventing, Identifying and Addressing Mental Health and Substance Abuse Issues in Youth (Topic Summary) (ccsa.ca)
- footnote[11] Back to paragraph School Mental Health Ontario
- footnote[12] Back to paragraph School Mental Health Ontario
- footnote[13] Back to paragraph School Mental Health Ontario
- footnote[14] Back to paragraph School and Community System of Care Collaborative. (2022). Right time, right care: Strengthening Ontario’s mental health and addictions system of care for children and young people
- footnote[15] Back to paragraph School Mental Health Ontario
- footnote[16] Back to paragraph Ontario Hospital Association. Measurement-Based Care in Mental Health: Why, How, and What?
- footnote[17] Back to paragraph Public Health Ontario (2021). Trauma-informed practices for children and families during the COVID-19 pandemic. Trauma-informed Practices for Children and Families - Publications Ontario (gov.on.ca)
- footnote[18] Back to paragraph Ministry of Education (2023). Considerations for program planning- Human Rights, Equity and Inclusive Education.