Government Notices Respecting Corporations
Certificate of Dissolution
Notice Is Hereby Given that a certificate of dissolution under the Business Corporations Act, has been endorsed. The effective date of dissolution precedes the corporation listings.
|
Date |
Name of Corporation |
Ontario Corporation Number |
|---|---|---|
|
2001-2-14 |
Linux Open Source Capital Canada, Inc. |
1395015 |
|
2001-3-2 |
L.S.S. Consulting (Canada) Inc. |
1174589 |
|
2001-3-2 |
Roger & Lois Harris Inc. |
748068 |
|
2001-3-8 |
770196 Ontario Inc. |
770196 |
|
2001-3-9 |
Associated Concrete Systems Ltd. |
752449 |
|
2001-3-9 |
Duncam Developments Limited |
233469 |
|
2001-3-9 |
Dyles Consulting Inc. |
1110917 |
|
2001-3-9 |
Jack E. Forrest & Associates Inc. |
958658 |
|
2001-3-9 |
Wescraw Aviation Inc. |
1127782 |
|
2001-3-12 |
Don Jackson Trucking Ltd. |
295299 |
|
2001-3-12 |
Madge Networks (Canada) Inc. |
1037475 |
|
2001-3-12 |
Mcmaster Communications Inc. |
1076352 |
|
2001-3-12 |
The Flooring & Design Centre (Windsor) Ltd. |
1383228 |
|
2001-3-12 |
Tomorrow Way Trading Inc. |
1095019 |
|
2001-3-13 |
Abel/Noser Inc. |
724663 |
|
2001-3-13 |
Deeb-Wallans Corporation |
765766 |
|
2001-3-13 |
H & Y Computer Corporation |
1173974 |
|
2001-3-13 |
Iaad Transportation Limited |
1375891 |
|
2001-3-13 |
Jssqui Holdings Limited |
872408 |
|
2001-3-13 |
M.A. Garment Inc. |
1418580 |
|
2001-3-13 |
Mad River Holdings Inc. |
872406 |
|
2001-3-13 |
Marketing Forces Inc. |
1380374 |
|
2001-3-13 |
Stan-Mar Corp. Ltd. |
872407 |
|
2001-3-13 |
The Bear’s Inn Inc. |
1245021 |
|
2001-3-13 |
1313105 Ontario Inc. |
1313105 |
|
2001-3-14 |
Amdix Holdings Inc. |
1058252 |
|
2001-3-14 |
Eurovail Healthcare Incorporated |
1061525 |
|
2001-3-14 |
Murrorah Inc. |
1245395 |
|
2001-3-14 |
Noviline Inc. |
978208 |
|
2001-3-14 |
692818 Ontario Inc. |
692818 |
|
2001-3-14 |
839214 Ontario Inc. |
839214 |
|
2001-3-14 |
1158492 Ontario Inc. |
1158492 |
|
2001-3-15 |
Kids Kan Bounce Inc. |
1303018 |
|
2001-3-15 |
1312446 Ontario Inc. |
1312446 |
|
2001-3-15 |
1321431 Ontario Inc. |
1321431 |
|
2001-3-15 |
1321432 Ontario Inc. |
1321432 |
|
2001-3-15 |
1378097 Ontario Limited |
1378097 |
|
2001-3-16 |
Internet Front Inc. |
1128343 |
|
2001-3-16 |
Lai’s Fruit & Vegetable Station Inc. |
1222818 |
|
2001-3-16 |
38 Trading Company Inc. |
1184148 |
|
2001-3-16 |
802913 Ontario Limited |
802913 |
B. G. Hawton
Director (A), Companies Branch
13/01
Notice of Default in Complying with the Corporations Information Act
Notice Is Hereby Given under subsection 241 (3) of the Business Corporations Act that unless the corporations listed hereunder comply with the filing requirements under the Corporations Information Act within 90 days of this notice orders dissolving the corporation(s) will be issued. The effective date precedes the corporation listings.
|
Date |
Name of Corporation |
Ontario Corporation Number |
|---|---|---|
|
2001-3-15 |
C.M.F.J. Corporation |
1082542 |
B. G. Hawton
Director (A), Companies Branch
13/01
Cancellation of Certificate of Incorporation (Corporations Tax Act Defaulters)
Notice Is Hereby Given that, under subsection 241 (4) of the Business Corporations Act, the Certificates of Incorporation of the corporations named hereunder have been cancelled by an order dated 5th March, 2001 for default in complying with the provisions of the Corporations Tax Act, and the said corporations have been dissolved on that date.
|
Date |
Name of Corporation |
Ontario Corporation Number |
|---|---|---|
|
2001-03-05 |
Perly Toronto Inc. |
674849 |
B. G. Hawton
Director (A), Companies Branch
13/01
Notice of Default in Complying with the Corporations Tax Act
The Director has been notified by the Minister of Finance that the following corporations are in default in complying with the Corporations Tax Act.
Notice Is Hereby Given under subsection 241 (1) of the Business Corporations Act, that unless the corporations listed hereunder comply with the requirements of the Corporations Tax Act within 90 days of this notice, orders will be made dissolving the defaulting corporations. All enquiries concerning this notice are to be directed to Corporations Tax Branch, Ministry of Finance, 33 King Street West, Oshawa, Ontario L1H 8H6.
|
Number |
Name of Corporation |
Ontario Corporation Number |
|---|---|---|
|
1 |
D.A. Debruyne Landscaping Inc. |
1000556 |
B. G. Hawton
Director (A), Companies Branch
13/01
Erratum Notice
Vide Ontario Gazette, Vol. 131-29 dated July 18, 1998.
The following corporation was dissolved in error under Section 7 (1) of the Extra-Provincial Corporations Act, and has reverted to active status.
|
Number |
Name of Corporation |
Ontario Corporation Number |
|---|---|---|
|
1 |
Friars Minor Of The Order Of St. Francis |
42446 |
B. G. Hawton
Director (A), Companies Branch
13/01
Ministry of Municipal Affairs and Housing
Social Housing Reform Act, 2000
Notice Of Determination Of The Minister Of Municipal Affairs And Housing With Respect To Federal Funding Payments To Service Managers FOR 2001, AND MINISTRY PROJECTIONS FOR 2002 - 2005
Notice Is Hereby Given pursuant to subsection 134(2) of the Social Housing Reform Act, 2000 that the Minister of Municipal Affairs and Housing has determined that the amount of federal funding payable by the Minister under subsection 134(1) to each service manager for the year 2001 shall be the amount set out in the following table in the 2001 column opposite the name of the service manager. This notice replaces the notice published on December 30, 2000. The amounts set out in the columns for 2002 to 2005 are Ministry projections of the amounts of federal funding payable to each service manager for those years, and are subject to the Minister’s determination under subsection 134(1) for each of those years. Note: Actual net payments will be adjusted and paid in accordance with the Social Housing Reform Act, 2000, including subsections 134(6) and (9), and 126(2).
|
Service Manager |
2001 |
2002 |
2003 |
2004 |
2005 |
|---|---|---|---|---|---|
|
Norfolk County |
1,352,350 |
1,360,524 |
1,368,789 |
1,370,256 |
1,331,581 |
|
City of Hamilton |
22,074,930 |
22,208,345 |
22,343,256 |
22,367,212 |
22,131,667 |
|
Regional Municipality of Niagara |
9,322,556 |
9,378,899 |
9,435,874 |
9,445,991 |
9,346,517 |
|
City of Ottawa |
29,988,817 |
30,170,062 |
30,353,339 |
30,385,883 |
30,065,895 |
|
Regional Municipality of Waterloo |
9,432,878 |
9,489,888 |
9,547,537 |
9,557,774 |
9,447,821 |
|
District Municipality of Muskoka |
987,483 |
993,451 |
999,486 |
1,000,558 |
990,021 |
|
County of Oxford |
1,619,074 |
1,628,860 |
1,638,755 |
1,640,512 |
1,623,236 |
|
City of Brantford |
3,057,426 |
3,075,905 |
3,094,590 |
3,097,908 |
3,065,285 |
|
County of Bruce |
1,040,845 |
1,047,136 |
1,053,497 |
1,054,626 |
1,043,520 |
|
County of Dufferin |
1,284,861 |
1,292,626 |
1,300,479 |
1,296,370 |
1,280,409 |
|
City of St. Thomas |
1,398,055 |
1,406,504 |
1,415,048 |
1,380,155 |
1,350,344 |
|
City of Windsor |
10,669,340 |
10,733,823 |
10,799,028 |
10,712,623 |
10,558,698 |
|
City of Kingston |
4,359,305 |
4,385,651 |
4,412,293 |
4,417,024 |
4,370,509 |
|
County of Grey |
1,707,660 |
1,717,981 |
1,716,888 |
1,713,854 |
1,675,740 |
|
County of Hastings |
3,937,528 |
3,961,326 |
3,985,390 |
3,959,165 |
3,893,841 |
|
County of Huron |
980,885 |
986,813 |
992,808 |
972,902 |
953,858 |
|
Municipality of Chatham-Kent |
2,420,941 |
2,435,572 |
2,450,368 |
2,452,995 |
2,427,163 |
|
County of Lambton |
1,956,581 |
1,968,406 |
1,980,363 |
1,982,487 |
1,961,609 |
|
County of Lanark |
1,367,111 |
1,375,373 |
1,383,728 |
1,385,212 |
1,370,625 |
|
United Counties of Leeds and Grenville |
1,762,633 |
1,773,285 |
1,784,058 |
1,783,000 |
1,762,977 |
|
County of Lennox and Addington |
721,956 |
726,319 |
730,731 |
731,515 |
723,811 |
|
City of London |
9,179,477 |
9,234,955 |
9,291,056 |
9,301,017 |
9,203,070 |
|
County of Northumberland |
1,472,395 |
1,481,293 |
1,490,292 |
1,491,890 |
1,476,179 |
|
City of Stratford |
1,528,616 |
1,537,855 |
1,547,197 |
1,548,856 |
1,525,759 |
|
City of Peterborough |
5,053,746 |
5,084,290 |
5,115,176 |
5,120,660 |
5,066,736 |
|
United Counties of Prescott and Russell |
1,742,488 |
1,753,019 |
1,763,668 |
1,765,559 |
1,746,966 |
|
County of Renfrew |
2,537,497 |
2,552,833 |
2,568,341 |
2,571,095 |
2,544,019 |
|
County of Simcoe |
7,545,920 |
7,591,526 |
7,637,642 |
7,610,806 |
7,515,962 |
|
City of Cornwall |
4,435,850 |
4,462,659 |
4,489,769 |
4,494,583 |
4,447,251 |
|
City of Kawartha Lakes |
1,864,785 |
1,876,055 |
1,887,452 |
1,866,377 |
1,837,031 |
|
County of Wellington |
3,583,062 |
3,604,717 |
3,626,615 |
3,630,504 |
3,592,272 |
|
Algoma District Services Administration Board |
1,505,589 |
1,514,688 |
1,523,890 |
1,525,524 |
1,509,459 |
|
District of Cochrane Social Services Administration Board |
4,994,008 |
5,024,191 |
5,054,711 |
5,060,131 |
5,006,844 |
|
Kenora District Services Board |
2,532,917 |
2,548,225 |
2,563,705 |
2,566,454 |
2,539,427 |
|
Manitoulin-Sudbury District Social Services Administration Board |
1,171,412 |
1,178,491 |
1,185,650 |
1,186,922 |
1,174,422 |
|
District of Nipissing Social Services Administration Board |
4,868,010 |
4,897,431 |
4,927,182 |
4,932,465 |
4,880,522 |
|
District of Parry Sound Social Services Administration Board |
815,489 |
820,418 |
825,402 |
826,287 |
817,585 |
|
District of Rainy River Social Services Administration Board |
1,634,923 |
1,644,804 |
1,654,796 |
1,656,570 |
1,639,125 |
|
City of Greater Sudbury |
8,417,919 |
8,468,795 |
8,520,241 |
8,529,376 |
8,439,555 |
|
District of Thunder Bay Social Services Administration Board |
10,231,139 |
10,292,974 |
10,355,502 |
10,328,648 |
10,203,953 |
|
District of Timiskaming Social Services Administration Board |
2,105,807 |
2,118,534 |
2,131,404 |
2,133,689 |
2,111,219 |
|
District of Sault Ste. Marie Social Services Administration Board |
4,734,166 |
4,762,778 |
4,791,711 |
4,796,849 |
4,746,334 |
|
Regional Municipality of Durham |
10,817,841 |
10,883,221 |
10,949,334 |
10,961,074 |
10,845,645 |
|
Regional Municipality of York |
9,346,829 |
9,403,319 |
9,460,442 |
9,470,586 |
9,370,852 |
|
City of Toronto |
170,492,660 |
171,491,176 |
172,522,337 |
172,707,313 |
170,888,563 |
|
Regional Municipality of Peel |
22,828,595 |
22,966,566 |
23,106,083 |
23,130,857 |
22,887,270 |
|
Regional Municipality of Halton |
4,726,911 |
4,755,479 |
4,784,367 |
4,789,497 |
4,739,060 |
Dated this 21st day of March, 2001
Chris Hodgson
Minister of Municipal Affairs and Housing
(6856) 13
Municipal Act
Order Made Under The Municipal Act R.S.O c.M.45
County Of Hastings
Village Of Marmora
Township Of Marmora And Lake
Change of Name for the Municipality of Marmora
The name of “The Corporation of the Municipality of Marmora” established under section 2 of the Order of the Minister of Municipal Affairs and Housing dated June 30, 2000, as published in the Ontario Gazette on July 15, 2000, is hereby changed to “The Corporation of the Municipality of Marmora and Lake”.
Dated at Toronto this 14th day of March, 2001.
Chris Hodgson,
Minister of Municipal Affairs and Housing.
(6857) 13
Financial Services Commission of Ontario
March 31, 2001
Professional Fee Guidelines – Psychologists
Professional Fee Guideline No. 3/01
Professional Fees Guideline - Psychologists
This guideline is issued pursuant to Subsections 14 (4), 15 (6), 17 (2) and 24 (2) of the Statutory Accident Benefits Schedule - Accidents on or After November 1, 1996 (Sabs) and applies to expenses incurred on or after March 31, 2001.
Purpose
This guideline sets out the maximum fee for the services of a psychologist that an insurer is liable to pay for:
- a medical benefit under Subsections 14 (2) (b) or (h) of the Sabs;
- a rehabilitation benefit under Subsections 15 (5) (a) to (g) or 15 (5)(l) of the Sabs; or
- conducting an examination or assessment or providing a certificate, report or treatment plan under Subsection 24 (1) (a) of the Sabs.
This guideline applies only to services rendered by psychologists.
Fees for Psychologists
The maximum hourly rate for services provided by a psychologist is $180.00 per hour effective until December 31, 2001.
The rate for ancillary personnel such as psychometrists is not covered by this guideline. The work of ancillary personnel will be separately identified on any invoice with the nature of the service provided and the hourly rate charged.
Psychology Assessment and Treatment Guidelines
Psychologists and insurers should also make reference to the Psychology Assessment and Treatment Guidelines separately published The Ontario Gazette on March 31, 2001 pursuant to Section 268.3 of the Insurance Act.
Professional Fee Guidelines - Speech - Language Pathologists
Professional Fee Guideline No. 2/01
Professional Fee Guideline - Speech-Language Pathologists
This guideline is issued pursuant to Subsections 14 (4), 15 (6), and 24 (2) of the Statutory Accident Benefits Schedule - Accidents on or After November 1, 1996 (Sabs) and applies to expenses incurred on or after March 31, 2001.
Purpose
This guideline sets out the maximum fee for the services of a speechlanguage pathologist that an insurer is liable to pay for:
- a medical benefit under Subsections 14 (2) (a) or (h) of the Sabs;
- a rehabilitation benefit under Subsections 15 (5) (a) to (g) or 15(5) (l) of the Sabs; or
- conducting an examination or assessment or providing a certificate, report or treatment plan under Subsection 24 (1) (a) of the Sabs.
This guideline applies only to reasonable and necessary services rendered by registered speech-language pathologists.
Fees for Speech-Language Pathologists
The maximum hourly rate for services provided by a speech-language pathologist is $135.00 per hour for professional time.
Psychology Assessment and Treatment Guidelines
Superintendent’s Guideline No. 2/01
Psychology Assessment and Treatment Guidelines
Application
These guidelines are issued pursuant to Section 268.3 of the Insurance Act.
These guidelines apply to psychological services provided to accident victims on or after March 31, 2001.
This document sets out assessment and treatment guidelines for use by psychological practitioners[1], insurers and insured motor vehicle accident victims. Part I of the document, the Psychology Assessment Guideline, defines an assessment and sets out maximum hours of assessment required prior to the application of the Treatment Guideline described in Part II.
Patient Groups Covered by the Treatment Guideline
The Treatment Guideline described in Part II is applicable only to treatment of the following groups of patients who, after assessment, are determined to have:
- Psychological impairments resulting from uncomplicated soft tissue injuries (Whiplash Associated Disorders (Wad) I, Ii, and Iii and Low Back Pain (Lbp), and pain; or
- Post-traumatic psychological stress reactions with no physical injuries or pain; or
- Psychological impairments resulting from uncomplicated soft tissue injuries (Wad I, Ii, and Iii) and pain, combined with posttraumatic psychological stress reactions.
Time Frame Covered by Treatment Guideline
As indicated in Part II, Tables 1-3, this guideline is intended to portray maximum psychological treatment for these three prevalent patient groups injured in motor vehicle accidents in the first three phases of treatment consistent with a phased model of psychological treatment:
- phase I, 0-6 weeks following initiation of treatment;
- phase Ii, 6-12 weeks following initiation of treatment and
- phase Iii, 12-24 weeks following initiation of treatment.
This guideline does not address any treatment phase beyond 24 weeks.
Patient Groups to Which Treatment Guideline Maximums Do Not Apply
The maximums in the treatment guideline do not apply to treatment of any patient presenting with the following characteristics:
- Risk of harm to self or others;
- Brain injury/ cognitive impairments;
- Other body injuries, for example, spinal cord injury, amputations, scarring, disfigurement;
- Children, adolescents and elderly;
- Contextual factors such as cultural and linguistic factors that may impede treatment progress. When reasonably available, assessment and treatment in the patient’s native language should be provided to patients with limited English;
- The MVA caused catastrophic injury or death;
- Patients with pre-existing severe psychological disorders;
- Patients with alcohol and substance abuse disorders.
These characteristics suggest more complex and intense treatment needs than contemplated for the groups specifically covered by the guideline.
Intended Use Of These Guidelines
If, in any individual case, a conflict arises between these guidelines and the Rules of Professional Conduct and Standards of Practice for Psychology, then the rules and standards governing the profession will prevail.
As the duration and number and severity of injuries/ conditions/ impairments and functional activity limitations/ participation restrictions increase so does case complexity and there is an accompanying infeasibility of relying on standardized guides to frame patient needs. For that reason, there is no attempt in this Guideline to deal with any condition requiring psychological treatment, any patient group, nor any time frame that falls outside the stated application.
These guidelines define maximum assessment in Part I: Psychology Assessment Guideline, and maximum psychological treatment for specified groups of patients for the first 24 weeks of treatment.
Presumed Pre-Approval for Treatment in Phase I
Where a psychological treatment plan contemplates treatment which falls within these guidelines, approval of proposed treatment may be presumed where the following procedure is adopted. Where presumed pre-approval applies, the psychologist will telephone the insurer to advise that a Treatment Plan is to be expected and then the Treatment Plan will be faxed to the adjuster and clearly marked, “For Rapid Response pursuant to the Psychology Guideline”. The insurer will communicate any objection to the Phase I treatment within 3 business days of its receipt.
If the insurer does not respond within 3 business days to a treatment plan presented in accordance with this guideline, it will be presumed to have insurer pre-approval for funding for Phase I, the first six weeks, and the insurer will pay for all expenses incurred after submission of the treatment plan in respect of the psychological services described in the treatment plan, for Phase I.
Any proposed treatment in the plan for a period beyond Phase I or six weeks, shall be dealt with according to the Sabs.
It is not intended that the Treatment Guideline would be used to replace or circumvent patient assessment, nor as a basis for refusing to pay for the cost of assessments pursuant to Section 24 of the Sabs. Assessment before treatment is still required.
Covered Patient Groups Defined
Group I: Patients with psychological impairments resulting from uncomplicated soft tissue injuries (Wad I, Ii, and Iii and Lbp) and pain
The first patient group addressed in these Guidelines includes patients with uncomplicated soft tissue injuries (Wad I, Ii, and Iii & Lbp), including psychological reactions to continuing pain and functional limitations from these injuries. These musculoskeletal disorders comprise the most prevalent patient groups arising from motor vehicle accidents. A subgroup of patients with these injuries may have debilitating pain and functional limitations/ restrictions leading to psychological impairments. Psychologists are trained both in treating directly the psychological impairments and in teaching pain management strategies that are effective in educating patients and their families and ameliorating the frustration-anger-pain cycle.
Continuing pain can give rise to a myriad of problems in social/family/marital or school/ occupational role functioning as well as secondary physical functioning problems such as deconditioning and weight gain. When pain impairments limit ability to function in school or occupational roles the patient may experience a significant disruption to their sense of self in addition to anxieties about their ability to maintain or regain their pre-accident life status. Social/family/marital disruption may occur with reduced participation with family or friends, as well as tendencies to avoidance and isolation. Increased irritability and difficulty controlling anger may be evident. Continuing pain and functional limitations/restrictions may also lead to adjustment, mood and anxiety disorders with affective, cognitive, and/or physiological symptoms. Sleep disorders with difficulties such as falling asleep, remaining asleep, or restless sleep are often reported and directly impact physical and emotional wellness. These psychological conditions may, in turn, cause further functional activity limitations/ participation restrictions.
Timely psychological treatment to address the pain and psychological impairments is indicated to maximize efficient, effective restoration of the patient to pre-accident functional levels. Failure to address psychological factors contributes to prolonged impairments, increased medical/rehabilitation costs, and continuing functional limitations/ restrictions. Later provision of psychological treatment, while often indicated and effective, may need to be more protracted due to the chronicity of the impairments and the development of secondary conditions.
Group II: Patients with post-traumatic psychological stress reactions with no physical injuries or pain
The second patient group addressed in this Guideline are those patients, with no bodily injuries or pain impairments, who have posttraumatic psychological stress reactions to the motor vehicle accident. Their psychological difficulties follow from the traumatic impact of the accident. Patients in this group present with a number of conditions such as: acute stress reactions, post-traumatic stress disorder, adjustment disorders, anxiety disorders, panic disorder, as well as specific phobias and disorders including passenger, driver and pedestrian anxiety.
Anxiety Disorders including Acute Stress Disorder (within one-month post MVA) or Post Traumatic Stress Disorder (Ptsd) may develop depending upon the patient’s experience of the threat to self or others of the accident. Patients may experience episodes of repeated reliving of the trauma in intrusive memories (“flashbacks”), dreams, or nightmares, and have a sense of “numbness” and emotional blunting.
Patients often show distress and avoidance of situations reminiscent of the trauma. Often patients experience motor vehicle anxiety as either driver/ passenger or a pedestrian. The anxiety may occur only in specific situations, or may generalize to other driving scenarios or to other non-vehicle situations which are experienced as threatening. There is usually a state of autonomic hyperarousal with hypervigilance, and enhanced startle reactions and insomnia. Anxiety and depression commonly co-occur. The onset of Ptsd follows the trauma with a latency period that may range from a few weeks to months.
Adjustment Disorders also occur in response to a traumatic experience of a motor vehicle accident. Patients with Adjustment Disorders present with states of subjective distress and emotional disturbance, usually interfering with social functioning and performance. The manifestations may vary and include depressed mood, anxiety or worry (or mixture of these), a feeling of inability to cope, plan ahead, or continue the present situation, as well of some degree of disability in the performance of daily routine. The predominant feature may be a brief or prolonged depressive reaction, or a disturbance of other emotions or conduct.
Psychological treatment of patients with these conditions fosters efficient, effective reduction of impairments and restoration of function.
Group Iii: Patients with psychological impairments resulting from uncomplicated soft tissue injuries (Wad I. Ii, and Iii) and pain, combined with post-traumatic psychological stress reactions
A third frequently treated patient group addressed in this Guideline, are those patients with a combination of the injuries/impairments in the first and second groups. This group of patients present with the most complex clinical situations addressed in this Guideline. These patients typically have more impairments and more functional limitations. The pain and trauma impairments often potentiate each other. It is necessary to address each of the impairments because of their interaction. Therefore, treatment of this group of patients is often more intensive than the other two groups of patients.
Assessment And Clinical Diagnosis Before Treatment
In all psychological treatment contexts, assessment must precede treatment. It is essential that the psychologist determine sufficient information about the patient’s condition and situation in order to prescribe treatment. The psychologist is required to provide the patient with: 1) the results of the assessment; and 2) the plan for treatment, including the goals to be addressed, anticipated benefits, the nature of the treatment, and the costs associated. With this information the patient is able to give informed consent to the proposed treatment. An exception would be urgent crisis intervention treatment required prior to completion of the full assessment.
The requirement of assessment and clinical diagnosis prior to treatment is consistent with direction from the College of Psychologists of Ontario, responsible for regulating the practice of Psychology in accordance with the Regulated Health Professions Act, as follows:
“A member evaluating a client’s treatment needs should ensure that enough information has been obtained to adequately assess the client’s psychological status to establish an appropriate treatment plan … a differential diagnosis (should) be established in order to develop a treatment plan appropriate to the client’s needs[2].”
Part I, Psychology Assessment Guideline, defines an assessment, provides a description of the assessment process and details associated costs.
The Sabs provide coverage for the reasonable cost of assessments in section 24.
Practitioners should make every effort to ensure that assessments are reasonable in the context of each individual case.
Insurers should honour claims for payment for assessments unless the insurer has reason to challenge the reasonableness of the fee claimed or assessment performed. Insurers are only obligated to pay for reasonable psychological assessment expenses. However, the reasonableness cannot be disputed solely on the basis that: the insurer did not request it, the insurer did not pre-approve it, or the insurer did not choose the provider.
Treatment Phases
Psychological treatment is proposed with time frames and goals and typically occurs in phases. In this Guideline three phases of treatment planning are described: 0-6 weeks, 6-12 weeks, 12-24 weeks. Treatment progress is evaluated through each phase and appropriate modifications made. Treatment typically is more intensive at the beginning and becomes less intensive toward the termination of treatment.
In some instances it may be indicated, to utilize a few sessions from the final phase at less frequent intervals in a “follow-up” phase for consolidation and relapse prevention as well as support for work/ school reintegration. When required, this “follow-up” may extend beyond the 24 weeks of treatment. However, the “follow-up” phase will not add additional hours or cost to the treatment described in this Guideline.
Treatment Required Past 24 Weeks Is Not Covered Or Excluded By These Guidelines
A subgroup of patients may require further phases of active treatment beyond the three phases described here. This Guideline has no application when active psychological treatment of longer than 24 weeks duration is required. In patient situations where active psychological treatment is needed for longer than 24 weeks, reference should be made to the provisions in the Sabs .
For patients with continuing conditions/disorders/impairments, and/or limitations/ restrictions of function, an assessment and treatment plan for further treatment should be completed as soon as it becomes clear to the treating psychologist that the patient will require active treatment beyond 24 weeks.
Clinical Progress Reviews, Consultation And Reporting
Clinical progress reviews are a component of clinical treatment (including re-administration of psychometric instruments if appropriate). A review should be completed after approximately every 6-8 sessions of treatment or as clinical need dictates to determine whether the patient is engaged in treatment and responding as anticipated and if modification is required to the treatment plan. The information from the review should be succinctly reported and copied to the insurer.
Communication
These guidelines, as with the development of a treatment plan under the regulations, work best in the context of open, timely, and ongoing communication between the patient, the insurer and the psychologist. It is the responsibility of all parties to foster this communication.
Part I: Psychology Assessment Guideline
The cost of assessments is based on the actual time spent completing the assessment. In applicable patient situations[3], the maximum cost will not be more than $2,700 for a general psychological assessment or $4,500 when a combination including neuropsychological, psycho-educational, or psycho-vocational assessments are included, but the amount of time spent on each intervention may vary from case to case. Psychological assessments reasonably include the following diagnostic interventions: Clinical Diagnostic Interview(s), Clinical Diagnostic Interview with collateral source, Psychological Testing, Review of External File Materials, Consultation, Documentation, and Feedback Interview. The amount of time spent on each diagnostic intervention will vary between assessments. This guide indicates the cost of the basic intervention of each type, plus “Extent Attributes” which are additional work required, depending on the individual factors of the case. Use of extent attributes increase the cost of that intervention. It is the responsibility of the psychologist who is completing the assessment to determine which interventions and extent attributes are reasonable and necessary. When required, cost of completion of the Ocf 18 is $75, and disbursements and travel time are additional.
|
Diagnostic Intervention &A; Cci |
Basic Hours[4] |
Cost[5] |
Plus Extent Attributes |
|---|---|---|---|
|
Clinical Diagnostic Interview(s) 2.Az.02 |
2.5 |
$450 |
Need for additional patient interviews. Increase time as per additional interview(s) e.g. further interview(s) required due to intellectual limitations/slowness, and/or to clarify complex history, causation, clinical presentation or multiple impairments. |
|
Clinical Diagnostic interview with collateral source 2.Az.02 |
Need for collateral interviews. Increase time as per additional interview(s) e.g. with family, teacher, employer |
||
|
Psychological Testing 2.Az.08 |
3 |
$540 |
Requirement for additional more extended specific test procedures to address outstanding diagnostic and impairment issues: Additional testing to elaborate findings from First Level: Clinical Health/ Rehabilitation testing- increase hours by 1-6 e.g. self- report inventories are inappropriate/insufficient; further testing RE: cognitive dysfunction, psychological dysfunction, behavioural disorder, competency evaluation. |
|
Review of External File Material |
1 |
$180 |
File contents beyond 50 pages: Increase by .25 hour for each additional 25 pages of documentation |
|
Consultation 7.Sf.12 |
Consultation with health professionals and the insurer required: Increase hours by 0.25 per consultation |
||
|
Documentation 7.Sj.30Zz |
4 |
$720 |
Complex situations which require more extensive data analysis and documentation. Actual time reasonably spent |
|
Feedback Interview 2.Az.02 |
1.5 |
$270 |
Complex situations which require additional diagnostic feedback interviews: increase time as per additional interview(s) e.g. patients with intellectual limitations/slowness or with severe and multiple psychological impairments may require additional feedback interviews |
Psycho-Educational/Psycho-Vocational Assessment
Assessment may include the following domains:
Intellectual abilities
Academic:
Reading
Writing
Numerical
Communication/Language:
Expressive
Receptive
Organizational and planning skills
Abstract Reasoning
Distractibility
Vocational aptitude
Vocational interests
Task skills analysis
Transferable skills
Endurance
Persistence
Adaptation and flexibility
Motivation
Achievement need
Learning
Personality
Emotional
Neuropsychological Assessment
Assessment may include the following domains:
Sensory abilities
Motor Skills
Psychomotor speed
Attention/Concentration
Language
Visuospatial/Constructional
Intellectual abilities
Memory and learning
Executive functioning
Judgment
Self awareness
Initiation
Self Control
Personality
Emotional
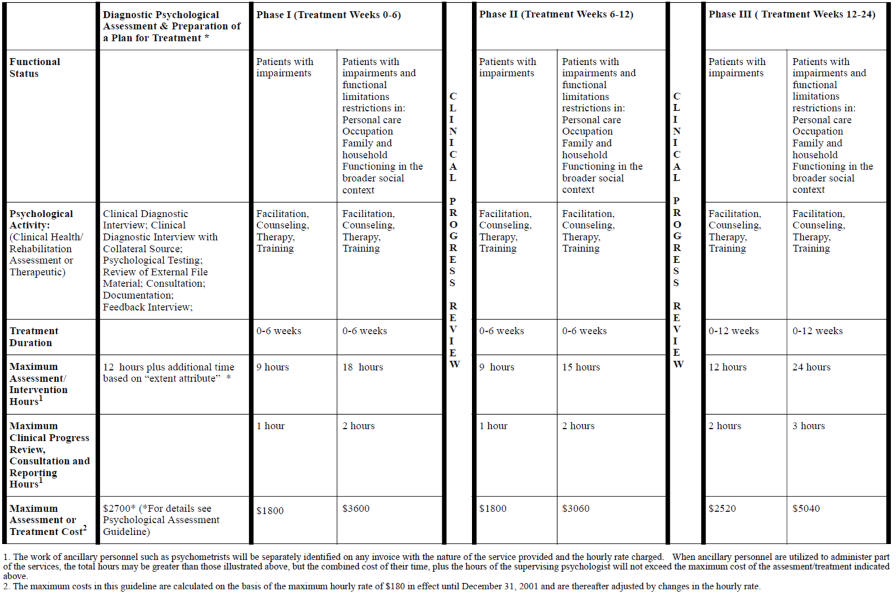
Part Ii: Psychology Assessment And Treatment Guideline
Table I: Patients with psychological impairments resulting from uncomplicated soft tissue injuries (Wad I, Ii, and Iii and Lbp) and pain
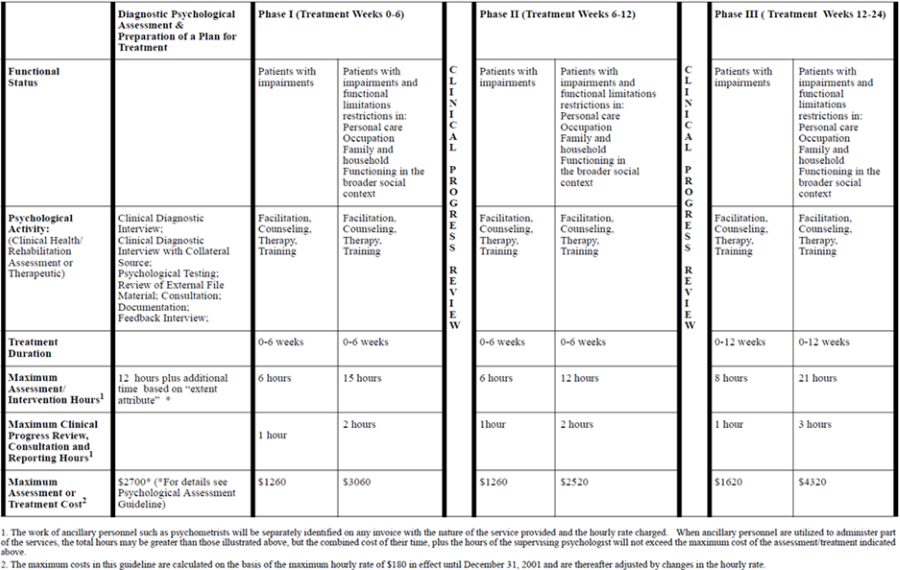
Table II: Patients with post-traumatic psychological stress reactions with no physical injuries or pain
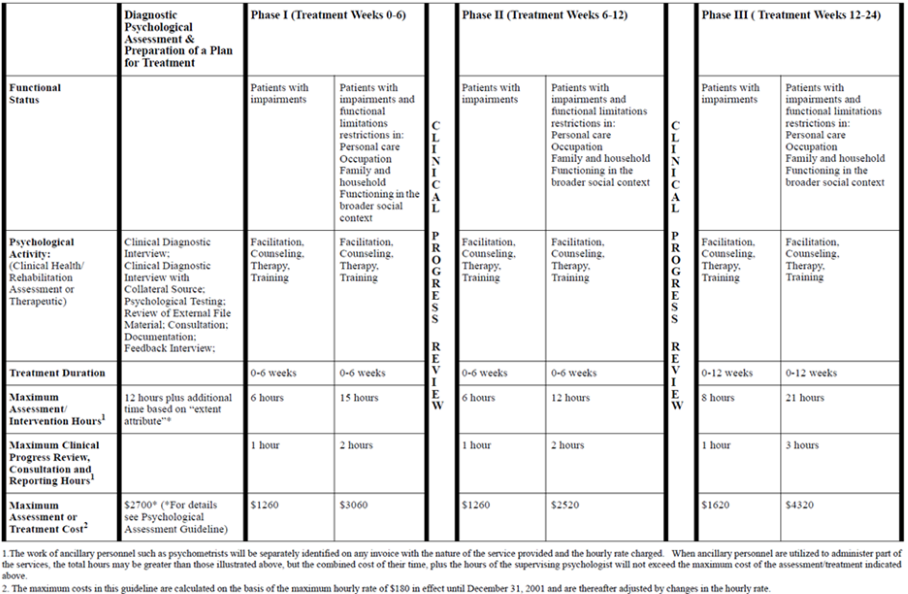
Table III: Patients with psychological impairments resulting from uncomplicated soft tissue injuries (Wad I. Ii, and Iii) and pain, combined with post-traumatic psychological stress reactions
Appendix I
Psychology Assessment And Treatment Guideline: Cci Definitions
The Canadian Classification of Interventions (Cci) provides the following descriptions of diagnostic interventions and extent attributes.
This coding system, with extent attribute modifiers, can be applied to the diagnostic interventions indicated in the Psychology Assessment and Treatment Guideline.
Extent attribute
Extent attribute is used to indicate, where appropriate, a quantitative measure related to the intervention (e.g. length of laceration repaired, number of anatomical structures involved).[6]
Clinical Diagnostic Interview
2.Az.02 Assessment, psychiatric, Includes: .
Assessment, criminal responsibility; Assessment, capacity for self harm; Assessment, capacity for violence; Assessment, financial competence; Assessment, cognitive status; Assessment, mental status; Determination, mental status (medicolegal, testamentary); Evaluation, forensic psychiatric;
Note: Involves diagnostic interview and evaluation. Code also: Any certification of psychiatric status or competency (see 7.Sj.30.^^)
2.Az.02.Zz, using technique NEC (“not elsewhere classified”)[7]
Psychological Testing
2.Az.08 Test, psychological, Includes:
Assessment, psychological (psychodiagnostic); Test, developmental (e.g. infant, intelligence); Test, psychometric; Test, reality;
2.Az.08.Yl, using visual technique (e.g. Bender, Benton);
2.Az.08.Ah, using inventory technique (e.g. Minnesota Multiphasic
Personality Inventory: Mmpi); 2Az.08.Aj, using memory scale technique (e.g. Weschler scale); 2.Az.08.Zz, using other technique
NEC (e.g. Bayley’s scale of infant development)
Review of External File Material
7.Sj.30Zz Documentation, support activity
Consultation
7.Sf.12.Planning, service (Includes: Conference, team; Planning, care; Planning, discharge; Programming, activity; Rounds, clinical service; Rounds, ward.
Documentation
7.Sj.30Zz Documentation, support activity, See above
Feedback Interview
2.Az.02 Assessment, psychiatric
OCF-18 Preparation
7.Sj.30Lb Completion, claim forms (e.g. insurance, third party payer, worker’s compensation)
Cci Definitions Of Interventions Used In Tables I, Ii, And Iii
Facilitation: Helping a client (by organizing, making arrangements, providing encouragement or supervision) to engage in activities that, for health reasons, would otherwise be impossible or very difficult to do independently.
Counseling: Providing health advice to a client that identifies health problems (or risks), encourages a change of client attitude or behaviour in order to initiate a willingness to modify lifestyle or behaviour that will result in an elimination of the health problem or risk.
Therapy: The general treatment of a condition, disease or dysfunction to eradicate its cause, manage or reduce the symptoms, or alleviate other associated disabling conditions by using appropriate selected techniques.
Training: Teaching new or different skills to assist a client in overcoming a functional problem (or impairment) that usually involves a complex learning process before those skills are acquired or integrated.
Appendix II
Classification Systems for Description of Injury, Impairments, Functional Activity Limitations/Participation Restrictions and Treatment
This Guideline is structured using two relevant classification systems: the ICD-10[8] for injury/disorder/condition and impairment description, and the Canadian Classification of Interventions (Cci)[9] for describing the treatment/intervention employed by the psychologist. These systems, rigorously developed, reviewed and revised on an ongoing basis, are in wide use both in Canada and internationally. The classification systems have been recommended for use in the Standard Invoice. Communication between practitioners, patients and insurers will be facilitated by the use of these same classification systems in the Assessment and Treatment Guideline.
Injury and Impairment Description and Multiaxial Clinical Diagnosis:
The International Statistical Classification of Diseases & Related Health Problems, Tenth Revision (ICD-10) has been developed by the World Health Organization (Who), with Canadian input coordinated by the Canadian Institute for Health Information (Cihi). The ICD-10 has been approved by the Conference of Deputy Ministers of Health as the new national standard for health problem classification (1999).
Psychologists generally employ a multiaxial approach to assessment, clinical diagnosis, treatment planning and provision of treatment/ rehabilitation. As stated in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, a classification system presently used by many psychologists, “The use of the multiaxial system facilitates comprehensive and systematic evaluation with attention to the various mental disorders and general medical conditions, psychosocial and environmental problems, and level of functioning that might be overlooked if the focus were on assessing a single presenting problem. A multiaxial system provides a convenient format for organizing and communicating clinical information, for capturing the complexity of clinical situations, and for describing the heterogeneity of individuals presenting with the same diagnosis.”
The ICD-10 also provides description of a multiaxial approach. While somewhat different from the Dsm Iv, using three rather than five axes, it incorporates the same conceptual approach and communicates generally similar information. In the ICD-10 system:
Axis I is the Clinical Diagnosis including: mental disorders, physical disorders, and personality disorders;
Axis II is used to describe any activity limitations/ participation restrictions in specific areas of functioning including: personal care; occupation; family and household; and functioning in the broader social context. Patients who are experiencing functional limitations/ restrictions in one or more of these domains, generally have more intense treatment needs;
Axis III is used to describe contextual factors, which are environmental and life style factors relevant to pathogenesis and course of the patient’s illness. The ICD-10 describes these influencing factors as relevant to patient description when, “some circumstance or problem is present which influences the person’s health status but is not in itself a current illness or injury… may be recorded as an additional factor to be borne in mind when the person is receiving care for some illness or injury” (ICD-10, Vol. 1).
This approach to patient description is consistent with how psychological practitioners provide assessment, diagnosis and treatment/rehabilitation to individual patients, i.e. they diagnose the disorders/conditions and impairments of physical and psychological function and describe any associated functional limitations/restrictions. The goals of treatment often include: treatment of the disorder/ condition; reduction of the impairment(s); restoration of functional ability; reduction or prevention of disability; and facilitation, in so far as possible, of a return to pre-injury normal life pursuits. The nature and intensity of the treatment must also take into consideration contextual factors.
In other words, the description communicates more than just a diagnosis that alone is often insufficient to describe the health problem. For example, two people with the same diagnosis will typically experience a different “impact” of the diagnosed condition on their lives, and will often have markedly different treatment/rehabilitation needs.
Patients with activity limitations/ participation restrictions generally have greater treatment/ rehabilitation needs. Each of the three Treatment Guideline tables further divides patients into two subgroups within each phase, those with only disorders/conditions/impairments and those with disorders/conditions/impairments causing functional limitations/restrictions in:
- personal care
- occupation
- family & household
- functioning in broader social context.
Those patients with only disorders/conditions/impairments require timely intervention to prevent development of functional limitations/ participation restrictions, while those patients who also have functional limitations/restrictions often require more intensive intervention. These varying levels of treatment are reflected in Tables 1-3 in Part II.
Intervention/Treatment Classification:
The Canadian Institute for Health Information (Cihi) is the developer of a new classification of interventions that will replace the existing “Canadian Classification of Diagnostic, Therapeutic and Surgical Procedures” (Ccp). The new classification system is referred to as Canadian Classification of Health Interventions (Cci). This multidisciplinary intervention classification system has been approved by the Conference of Deputy Ministers of Health as the new national standard for health problem classification (1999). The interventions described in the CCI, also correspond to the descriptions provided in the Schedule of Services, Guide to Fees and Billing Practices, Ontario Psychological Association, 1988.
Transportation Expense Guidelines
Superintendent’s Guideline No. 3/01
Transportation Expense Guidelines
These guidelines are issued pursuant to subsections 14(5), 15(11) and 24(3) of the Statutory Accident Benefits Schedule - Accidents on or After November 1, 1996 (Sabs) and section 268.3 of the Insurance Act. These guidelines replace Guideline No. 6/96 effective March 31, 2001.
Purpose
The purpose of the Transportation Expense Guidelines is to provide a framework for insurers and insured persons to determine the circumstances under which expenses related to transportation of an insured person to and from treatment sessions must be paid by an insurer. The guidelines set out authorized expenses and applicable rates for the purpose of subsections 14(5), 15(11) and 24(3) of the Statutory Accident Benefits Schedule - Accidents on or After November 1, 1996.
Authorized Expenses
The insurer is liable to pay for all reasonable and necessary transportation expenses for each trip that the insured person makes to and from treatment sessions, counselling sessions, training sessions, examinations and assessments. The insurer is also liable to pay for all reasonable and necessary transportation expenses of the insured person’s aide or attendant. Transportation expenses are calculated based on the most direct route. Transportation expenses include parking fees incurred.
The mode of transportation selected should be the most economical, practical for the distance to be travelled and appropriate under the specific circumstances.
Use of Automobiles
The insurer is liable to pay a mileage expense for transportation of the insured person and their aide or attendant, to and from treatment sessions, counselling sessions, training sessions, examinations and assessments using the insured person’s automobile, excluding the first 50 kilometres of each round-trip. The 50 kilometre “deductible” is only applicable once in any round-trip. This applies to minors who are driven to treatment sessions, examinations or assessments.
For the purpose of these guidelines, the “insured person’s automobile” includes any automobile owned or leased by the insured person or any other automobile to which the insured person has access.
The rate that is to be used to calculate transportation expenses for the use of the insured person’s automobile is 27.5¢ per kilometre (27.5¢/ km) travelled
Use of Taxis
The insurer is liable to pay for reasonable and necessary taxi fare incurred by an insured person and their aide or attendant provided that,
- the insured person does not own or have access to an automobile;
or
- the insured person is unable to operate an automobile; or
- it is reasonable and practical in the circumstances to take a taxi.
Other Modes of Transportation
Insurers are liable to pay for reasonable and necessary expenses for other modes of transportation where circumstances warrant. Before an insured person incurs expenses for air, rail and bus transportation services, he or she should discuss the matter with their insurer.
(6858) 13
Financial Services Commission of Ontario
RE: Financial Services Commission of Ontario Priorities — Request for Submissions
The Financial Services Commission of Ontario Act, 1997 (FSCO Act) requires the Financial Services Commission of Ontario to deliver to the Minister of Finance, and publish in The Ontario Gazette, a statement setting out the proposed priorities of the Commission for the following fiscal year in connection with the administration of the Insurance Act, the Compulsory Automobile Insurance Act, the Motor Vehicle Accident Claims Act, the Marine Insurance Act, the Prepaid Hospital and Medical Services Act, the Co-operative Corporations Act, the Credit Unions and Caisses Populaires Act, the Loan and Trust Corporations Act, the Mortgage Brokers Act, the Pension Benefits Act and the Registered Insurance Brokers Act, together with a summary of the reasons for the adoption of those priorities.
The statement of priorities for the coming fiscal year will be submitted to the Minister of Finance in June 2001 and will be published in The Ontario Gazette shortly thereafter.
In keeping with the FSCO Act and the Commission’s goal of furthering transparency in the regulatory process, the Commission invites interested parties to make written submissions regarding their views as to the matters that should be identified as priorities of the Financial Services Commission of Ontario.
For a copy of the Statement of Priorities, or to forward submissions by April 30, 2001, please contact:
Chief Executive Officer and Superintendent of Financial Services
Financial Services Commission of Ontario
5160 Yonge Street, Box 85
Toronto, Ontario M2N 6L9
or fax to (416) 590-7070.
(6862) 13
[1] Sabs define a psychologist as a person authorized by law to practice psychology. This includes Psychologists and Psychological Associates.
[2] The Bulletin The College of Psychologists of Ontario, Providing Psychological Services to Victims of Motor Vehicle Accidents: Considerations and Cautions, Vol 22 (3) Mar 1997.
[3] This Guideline does not apply to a patient who is a child, has a pre-existing severe psychological disorder, has a significant communication disorder or limited English (when reasonably available, patients should be assessed by a psychologist speaking the patient’s native language).
[4] The work of ancillary personnel such as psychometrists will be separately identified on any invoice with the nature of the service provided and the hourly rate charged. When ancillary personnel are utilized to administer part of the assessment, the total hours may be greater than those illustrated above, but the combined cost of their time, plus the hours of the supervising psychologist will not exceed the maximum cost of the assessment indicated above.
[5] The maximum costs in this guideline are calculated on the basis of the maximum hourly rate of $180 in effect until December 31, 2001 and are thereafter adjusted by changes in the hourly rate.
[6] Extent Attribute is used in Psychology Assessment Guideline to describe the assessment required for treatment plan preparation to indicate extension and further work and time units required in the component activity, for example, further specific psychological testing.
[7] The Opa has been informed by Canadian Institute for Health Information (Cihi) that the description of this activity is being amended to include clinical diagnostic interviews completed by psychologists.
[8] International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; World Health Organization, 1993 Geneva.
[9] Canadian Classification of Interventions