Results: Data and statistics
Register of pathologists
Under the Coroners Act, the Chief Forensic Pathologist (CFP) maintains a Register of Pathologists who are qualified to provide medicolegal services under the Act. Based on their qualifications and the recommendations of the credentialing subcommittee of the Forensic Pathology Advisory Committee (FPAC) registered pathologists are assigned a category that corresponds to the medicolegal services they can provide, including:
- all medicolegal autopsies, including homicide and criminally suspicious cases (Category A)
- routine cases only (Category B)
- non-suspicious paediatric cases (Category C)
During the reporting period, 88 registered pathologists were active in Ontario, including 38 Category A pathologists who are recognized as having additional experience, training and/or certification in forensic pathology.
Pathologists are registered for a five-year term, after which their appointments are considered for renewal. The quality team assembles data for review by the Credentialing and Continuing Professional Development Committee including:
- case load, cumulative over five years and year-by-year
- turnaround time for autopsy reports
- peer review history
- complaints, incident reports and critical incidents and remediation by the CFP and by the CPSO, where applicable
The CFP is responsible for the quality of medicolegal autopsies performed throughout the province. When there is professional misconduct or incompetence the CFP is legislatively obligated to report any registered pathologist to the CPSO. Similarly, the CPSO is obligated to inform the CFP of any issues with a registered pathologist.
Chart 2: Register Composition by Pathologist Category, 2010–2022
Summary:
(A/B/C)
- 2010–11: 24/142/5
- 2011–12 27/132/7
- 2012–13: 29/115/7
- 2013–14 31/99/7
- 2014–15: 31/97/7
- 2015–16: 34/66/6
- 2016–17: 39/65/7
- 2017–18: 40/66/7
- 2018–19: 41/70/9
- 2019–20: 40/73/8
- 2020–21: 40/68/6
- 2021–22: 38/45/5
Supervision and direction of pathologists
To promote consistent and high-quality practices across Ontario and support registered pathologists, the OFPS provides a practice manual and toolkit. The practice manual includes the Code of Ethics, practice guidelines for medicolegal autopsies and explanations of the quality assurance program and Register. Together, these documents provide the professional and policy foundation for the OFPS. The Code of Ethics was adapted from the Forensic Pathology Section of the Canadian Association of Pathologists.
Pathology Information Management System (PIMS)
The OFPS uses PIMS to collect information about autopsies performed across Ontario. All registered pathologists contribute information to the system through the Postmortem Examination (PME) record. This record is completed and submitted electronically to the OFPS after each autopsy. The record is reviewed daily by pathology administrators to ensure that autopsies are done according to guidelines. The collected information is also used to evaluate resources, as well as provide statistics about performance and quality.
Caseload statistics
Caseload statistics are derived from PME records submitted during the reporting period.
Each OFPS case begins with a coroner’s request for an autopsy through a warrant to a pathologist. All complex medicolegal autopsies, including homicide, criminally suspicious and paediatric cases, are performed in FPUs by appropriately qualified forensic pathologists. Routine cases are conducted at the FPUs and community hospitals. Some non-suspicious (medical-type) paediatric cases are performed at paediatric sites. In 2021–2022, 87.19 per cent of all autopsies were performed in FPUs and paediatric sites, and 12.80 per cent in community hospitals.
Chart 3 shows the distribution of autopsies performed at FPUs and community hospitals from 2021–2022.
Chart 3: Distribution of Autopsies at FPUs and Community Hospitals, 2021–2022
Summary:
- PFPU: 6184 (59.60%)
- Community Hospitals: 1328 (12.80%)
- Ottawa FPU: 1024 (9.87%)
- London FPU: 796 (7.67%)
- Sudbury FPU: 534 (5.15%)
- Kingston FPU: 354 (3.41%)
- Sault Area FPU: 155 (1.49%)
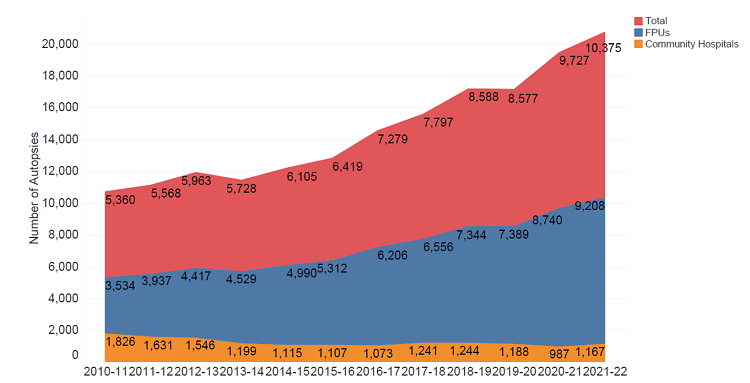
Chart 4 shows the distribution of autopsies performed at FPUs and community hospitals by year.
Chart 4: Distribution of Autopsies by Year, 2010–2022
Summary:
(Total/FPUs/Community hospitals)
- 2010–11: 5360/3534/1826
- 2011–12: 5568/3937/1631
- 2012–13: 5963/4417/1546
- 2013–14: 5728/4529/1199
- 2014–15: 6105/4990/1115
- 2015–16: 6419/5312/1107
- 2016–17: 7279/6206/1073
- 2017–18: 7797/6556/1241
- 2018–19: 8588/7344/1244
- 2019–20: 8577/7389/1188
- 2020–21: 9727/8740/987
- 2021–22: 10375/9208/1167
Paediatric autopsies (for children five years and under {DU5}) are often complex, requiring additional ancillary testing and/or consultation with other medical specialists. All paediatric autopsies of a criminally suspicious nature are performed in FPUs.
In 2021-22, there were a total of 166 paediatric cases (routine and criminally suspicious) completed across the province (Chart 5).
Chart 5: Paediatric Cases Involving Children under 5 Years by Locations, 2021–2022
Summary:
- PFPU: 78
- Community Hospitals: 32
- Ottawa FPU: 27
- London FPU: 24
- Sudbury FPU: 5
Chart 6 provides a breakdown of autopsies by case type for 2021–2022.
Chart 6: Distribution of Autopsies by Case Type, 2021–2022
Summary:
- Routine: 8285
- External: 1556
- Homicide: 273
- Death Under 5: 147
- Suspicious: 115
In some cases, the decision is made to limit an autopsy to an external examination where sufficient information can be obtained without dissection. There were 1,556 such cases performed at the OFPS in 2021–2022.
Forensic pathologists at the PFPU use imaging technology (such as CT scans) as a tool to inform their decisions about targeted examinations, where one or more body cavities are examined. In 2021–2022, 51 per cent of cases were targeted examinations (Chart 7).
Chart 7: Distribution of Autopsies by Autopsy Type in PFPU, 2021–2022
Summary:
- Targeted: 51%
- Full: 29.1%
- External: 19.8%
Quality management
The OFPS has a robust quality assurance program comprised of the following:
- the OFPS Register/pathologist credentialing
- practice guidelines, including standardized reporting templates and forms and standard operating procedures available in compliance management software
- consultation between pathologists in difficult or challenging cases
- reporting of key performance indicators to clients and stakeholders
- collection of standardized case information through the PME Record
- peer review of all autopsy reports on homicide, criminally suspicious, SIU cases and complex paediatric cases (deaths under five years) prior to report dissemination, including special peer review committees (Note: The Special Investigations Unit civilian oversight agency responsible for investigating circumstances involving police that have resulted in a death, serious injury, or allegations of sexual assault of a civilian in Ontario.)
- Child Injury Interpretation Committee (CIIC) for paediatric deaths
- Complex Case Expert Committee (CCEC) for complex cases
- quality reviews of reports related to routine autopsy cases
- peer review of courtroom testimony and/or transcript review
- detection and follow-up on significant quality issues and critical incidents
- tracking of complaints to ensure timely resolution and corrective action
- continuing medical education in forensic pathology:
- to maintain specialist competency as required by the Royal College of Physicians and Surgeons of Canada
- for continuing professional development
Peer review of autopsy reports for homicide, criminally suspicious, paediatric and SIU cases
There were 386 autopsy reports peer reviewed in 2021–2022. On average, about 12 reviews were completed by each reviewing forensic pathologist. The average turnaround time for peer review was seven days in 2021–2022. The OFPS standard for peer review is 10 working days.
Peer review of courtroom testimony by forensic pathologists
Forensic pathologists who testify as expert witnesses are required to submit one transcript of courtroom testimony each year for review by another forensic pathologist. Courtroom testimony is assessed for:
- preparedness
- qualifications (the testifying pathologist has the appropriate level and sphere of expertise)
- presentation style (responses to questions in chief and cross examination are appropriate in tone, length and thoroughness)
- knowledge (responses to questions are scientifically sound)
- interpretation/opinion/conclusions (credible and objective with strengths and limitations fairly presented)
- general comments on the registered pathologist’s court testimony
Seventeen courtroom testimonies were reviewed in the reporting period.
Quality review of autopsy reports for routine cases
Autopsy reports on routine cases (that is, non-criminally suspicious) are reviewed for administrative and technical accuracy by FPU Medical Directors and Medical Managers.
The administrative review focuses on completeness and adherence to guidelines. All community hospital reports undergo administrative review by the OFPS Quality Assurance Unit, and 10 per cent of routine autopsy reports from FPUs are reviewed by the Medical Director or Medical Manager.
The technical review focuses on the content of the report to ensure that the approach, conclusions and opinions derived from the evidence are reasonable and appropriate. In general, 10 percent of routine reports are reviewed on this basis.
A technical review is performed for all reports that fall into the following categories:
- cases with an undetermined/unascertained cause of death
- non-traumatic and non-toxicologic deaths of individuals younger than 40 years old
- reports from pathologists performing fewer than 20 medicolegal autopsies per year
- where the Quality Assurance Unit is notified that the case should undergo a mandatory technical review
Key performance indicators (KPIs)
KPIs for autopsy reports, such as submission compliance, completeness, consistency and turnaround time, are collected through the administrative and technical reviews and reported.
Table 1 shows the indicator, target outcome and overall performance for FPU and community hospital pathologists from 2021–2022.
Table 1: Key Performance Indicators for Autopsy Reports, 2021–2022
| Key Performance Indicators for Autopsy Reports | Target | Results |
|---|---|---|
| Submission Compliance (PME Record) | 100% | 96.5% |
| Completeness | 95% | 99.9% |
| Consistency | 95% | 99.9% |
| Turnaround Time (Turnaround time may be influenced by case complexity and availability of ancillary testing) | 120 days | Average = 93 days |
| Reports with Significant Issues (Forensic Pathology Units) | less than 2% | 0% |
| Reports with Significant Issues (Community Hospitals) | less than 2% | 2.1% (15 amended reports requested out of 720 audits) |
| Critical Incidents | 0 | 0 |
Pathologists are expected to follow the best practices set out in the practice manual. Pathologists are provided feedback from routine quality reviews with the goal of improving report quality.
Note: Community hospitals may use their own institution’s report templates if they include the required template fields.
Chart 8 illustrates consistency of the content and opinion of autopsy reports as assessed by the reviewing pathologist during the period, as shown by a technical review.
Chart 8: Consistency Measures as Shown by Technical Review, 2021–2022
Summary:
- Appropriate Ancillary Testing: FPUs 100.0%; Community Hospitals 100.0%
- COD Reasonable: FPUs 99.4%; Community Hospitals 96.9%
- Free of Language Errors: FPUs 99.4%; Community Hospitals 99.3%
- Independently Reviewable: FPUs 100.0%; Community Hospitals 100.0%
- Opinions are Reasonable: FPUs 99.4%; Community Hospitals 99.3%
- Satisfactory Descriptions: FPUs 100.0%; Community Hospitals 98.3%
Significant quality issues
Significant quality issues include substantial errors, omissions and other deficiencies.
A critical incident is a significant quality issue that contributes to a serious error in a death investigation. All critical incidents are analyzed to determine the root cause(s) and the corrective action that needs to be implemented to prevent future errors. There were no critical incidents for the reporting period.
If the reviewing forensic pathologist detects a significant quality issue during the technical review, feedback is provided to the case pathologist. For the given reporting period, there were no significant quality issues detected in routine case reports from FPUs or community hospitals.
The purpose of quality assurance is to improve the quality of autopsies and reports. When a significant quality issue is detected, the reviewing pathologist contacts the original pathologist directly to discuss and recommend changes to the report. Continued improvement of autopsy practice and report writing is supported with:
- ongoing education events such as the Annual Education Course for Coroners and Pathologists and special workshops on autopsy practice
- resources, such as the Practice Manual for Pathologists and Toolkit, including synoptic reports, annotated autopsy report templates and guidance with case examples from senior pathologists.
Turnaround time
Timeliness of autopsy reports is a key performance indicator. Turnaround time is influenced by case complexity, return of ancillary test results, pathologist workload and staffing levels. The OFPS standard regarding turnaround time is:
- 90 per cent of autopsy reports are to be completed within 120 days of the day of the autopsy
- cases involving homicides, paediatric deaths, deaths in custody and those in which the coroner has requested that the report be prioritized (due to requests from family or other parties) are to be expedited as a matter of routine
- no more than 10 per cent of cases should be greater than six months old without a justifiable reason for delay (for example, awaiting results of ancillary testing)
Chart 9 depicts the turnaround time for community hospital pathologists and forensic pathologists in FPUs for the last 12 years. The longer turnaround time for forensic pathologists may be explained by the more complex nature of the autopsies performed.
Chart 9: Average Turnaround Time, 2010–2022
Summary:
Average turnaround time by location and years
- 2010–11: Community Hospitals 85; FPUs 165
- 2011–12: Community Hospitals 55; FPUs 91
- 2012–13: Community Hospitals 66; FPUs 121
- 2013–14: Community Hospitals 75; FPUs 121
- 2014–15: Community Hospitals 67; FPUs 99
- 2015–16: Community Hospitals 72; FPUs 101
- 2016–17: Community Hospitals 75; FPUs 115
- 2017–18: Community Hospitals 100; FPUs 112
- 2018–19: Community Hospitals 100; FPUs 117
- 2019–20: Community Hospitals 82; FPUs 107
- 2020–21: Community Hospitals 93; FPUs 101
- 2021–22: Community Hospitals 80; FPUs 94