Program elements
Overview
The following section details the program elements that, when delivered sequentially, provide a continuum of service delivery for a child/youth and their family. Each element is informed by clinical evidence and best practices that can be used to support quality delivery of services. When available, Ontario examples are provided to help service providers implement these guidelines.
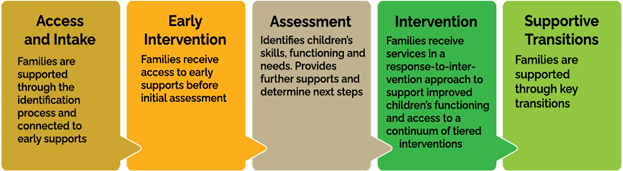
Image of five different coloured boxes that are side-by-side.
- Access and Intake: Families are supported through the identification process and connected to early supports
- Early Intervention: Families access to early supports before initial assessment
- Assessment: Identifies children’s skills, functioning and needs. Provides further supports and determines next steps.
- Intervention: Families receive services in a response-to intervention approach to support improved children’s functioning and access to a continuum of tiered interventions.
- Supportive Transitions: Families are supported through key transitions.
Access and Intake
Easy and early access is a key feature of the PSL and Children’s Rehabilitation Services programs. Helping families to connect to services early in a child’s developmental journey will contribute to improved outcomes and decrease the need for more intensive interventions later in life.
Access to Information
Access to evidence-informed and timely information about services is fundamental to a family’s ability to access services, make informed decisions, and to connect to other services they need.
In partnership with SmartStart Hubs,
Developmental monitoring supports healthy early development by building family and sector knowledge of developmental milestones and the capacity to detect risks or potential difficulties at the earliest point to eliminate or reduce the need for more intensive interventions at later stages.
Access to information and connection with service providers should be facilitated through a well-publicized and easy to access toll-free telephone number and email, website and social media. Families should be able to find information easily via many different sites and sources throughout the catchment (e.g., service provider locations, SmartStart Hubs, EarlyON Child and Family Centres and childcare settings, health services, AccessOAP and Autism Spectrum Disorder (ASD) Diagnostic Hubs).
Making resources available in clients’ first languages is one component of creating accessible and culturally safer services. Resources must be available in English and French at a minimum and in other languages, as needed. For example, if service providers identify the most common languages spoken in their catchment areas, they can consider translating print materials into those languages, attempting to hire staff who speak those languages, or learning about different connotations common English words may have in those languages. In all cases, an interpreter should be offered to families where required. Some families may choose to make their own arrangements for an interpreter (e.g., family member or friend); for others, the service provider should arrange for an interpreter (either in-person or remotely).
Access to Services
Families can self-refer
Families can initiate referrals on their own or provide consent to a service provider (including SmartStart Hubs), primary care provider, or an early years or education professional to initiate a referral. In some areas, new processes may be required to support parent self-referral and may result in changes to roles and responsibilities in the catchment, particularly for services for school-aged children. For example:
- In regions where SBRS referrals have typically been made through schools, CTCs should collaborate with District School Boards in their catchment to develop local processes to support referrals from all sources, including those made directly by families, enabling access to service provision in a variety of settings (home, school and community), as needed. See Collaboration and Partnerships.
- In circumstances where exceptional specialty services such as otolaryngology, feeding, or mobility clinics are needed in Children’s Rehabilitation Services, families can initiate contact with service providers, who can then support them to collect physician or regulated health professional referral documentation that may be necessary.
No diagnosis is required
Families do not need a diagnosis to access the PSL Program and/or Children’s Rehabilitation services and a diagnosis will not prevent access to services.
Coordinating intake processes within the catchment supports a more seamless and streamlined experience for families, facilitates access, and promotes equitable services.
SmartStart Hubs
SmartStart Hubs serve families with concerns about their child’s development and/or day-to-day functioning who would benefit from an exploratory discussion about their child’s strengths and support needs. Service providers are strongly encouraged to coordinate intake functions in their catchment, including with SmartStart Hubs, and other community entry points (e.g., Infant and Child Development Program).
See the SmartStart Hubs Policy and Practice Guidelines for more information about partnership expectations, including formal agreements between SmartStart Hubs and PSL Program providers.
Service provider intake process
When families enter services through SmartStart Hubs, intake processes for the PSL Program and Children’s Rehabilitation Services should build on information gathered by the Hub and shared with consent.
When families enter services directly through a local service provider, streamlined service pathways are enabled through intake processes that:
- Collect basic information and determine families’ developmental concerns and needs, including potential referral to a SmartStart Hub as informed by local agreements and protocols.
- Obtain consent to share relevant information to facilitate connections to a SmartStart Hub or other programs before initial assessment, as applicable.
- Connect families directly to other programs and services by sharing relevant information so that families don’t have to re-tell their stories, informed by local agreements and protocols.
- Connect families to Tier 1/Universal services so families receive information and support earlier (e.g., developmental milestones, home strategies; see Early Intervention for more information).
- Determine triage/prioritization approaches as needed (in cases where clinical service pathways may begin at intake) and as per local processes to:
- Respond to families with urgent or immediate needs (e.g., safety issues, equipment needs).
- Determine the type of assessment needed, as applicable (e.g., single or multi-disciplinary assessment; brief/rapid assessment).
- Note: In PSL, preschool-aged children with permanent hearing loss should follow the Infant Hearing Program clinical service delivery pathway from intake (as per the Infant Hearing Program Guidance Document).
What’s Happening in Ontario
Some regions use a common intake process across education, health, and community providers to streamline the family experience.
Many providers use online intake forms that support direct access to the appropriate service provider in the region, depending on identified needs.
Early Intervention
Early access to information improves the family experience and helps families build knowledge and skills to foster their children’s development, function, and participation. Having access to supports early may also alleviate anxiety and strengthen the family’s relationship with the service provider in preparation for additional services. Providing supports and services early helps to shift the conversation from “What can I do while I wait?” to “What can I do now to help my child’s development?” so that families are engaged in supporting their children’s needs and empowered to implement strategies at home right away.
Tier 1 supports will be accessible and beneficial to all, and registration will not be required for access. Tier 1 supports foster all children’s development and assist in identifying children in the community or education settings who may need additional supports, which can mitigate the need for further services.
In the context of PSL and Children’s Rehabilitation Services, Tier 1/Universal Intervention will involve:
- Actively developing knowledge and skills among families in service by providing general resources and support options directly to families before their initial assessment.
- Working collaboratively with partners as part of the service system to build capacity in education and community settings towards supporting and monitoring child development, identifying needs, implementing strategies, and connecting families with information and services.
Tier 1/Universal Supports
As part of Tier1/Universal supports, families will be connected to a range of early supports, including provincial family-based supports
There are a range of resources, information and tools that can help build families’ knowledge and skills so they can support their children’s development at home and prepare them for future services. These may include:
- General information so families can monitor their child’s development and identify needs and strengths.
- Information about how parents can engage as partners in service delivery or connect with other families for peer support.
- Home strategies so families can support their child’s abilities, functioning, and participation at various ages and stages, with a focus on every-day, natural routines and contexts.
In the context of PSL and Children’s Rehabilitation Services, Tier 1/Universal Supports will involve:
- Actively developing knowledge and skills among families in the service pathway by providing resources and supports before their initial assessment (e.g., links to webinars at intake to learn how to support their children’s needs at home).
- Working collaboratively with partners as part of the service system to build reciprocal capacity in education and community settings towards supporting child development, identifying needs, implementing strategies, and connecting families with information and services (e.g., providing language modelling strategies to early childhood educators to use with toddlers in childcare settings or in consulting collaboratively with educators regarding a learning environment in Children’s Rehabilitation Services).
These activities should also intersect with local early identification efforts and use of early identification resources that support and monitor growth and development in communities (see Appendix 5: Tiered Service and case examples).
In keeping with the principles of child- and family-centredness, Tier 1/Universal supports should be family-friendly, beneficial for all, and include different options so families can choose the resources, tools, and modalities that best meet their needs. Resources should consider diverse family needs, literacy levels, and consist of a variety of tools and supports in different formats.
At a minimum, these resources should be publicly accessible on service provider websites. Though most families may access resources electronically, service providers should ask families for their preferences, and other options should be available if needed (e.g., by mail, pick-up, distribution through another supportive agency).
Parents/caregivers should be encouraged to share Tier 1/Universal resources with other family members, childcare providers, educators, and others to help those involved in the child’s life to build knowledge and skills.
Community Partnerships
Community awareness initiatives that support early intervention should include reciprocal engagement and knowledge sharing with key service providers that interact with children, youth, and their families.
Key elements of building community knowledge and skills include:
- Training and education about universal strategies to support child development (e.g., webinars, workshops). This could include collaborating with other service partners, such as providing a workshop to EarlyON facilitators or inviting a childcare provider to attend parent training along with families.
- Providing coaching in early years settings or school settings which may include direct modelling of appropriate strategies and building educators’ capacities to support all children.
footnote 38 - In school settings, strategies must be in alignment with PPM 149 and/or with educator agreement.
- Establishing mechanisms to collaboratively observe, identify, and support children and connect families to other services when universal services do not seem to be sufficient, and the child has not yet been referred.
footnote 39
What’s happening in Ontario?
In some regions, families can sign up for email notifications or newsletters that provide information, resources, and access to webinars. This provides families with ongoing Tier 1/Universal intervention options before the initial assessment and beyond.
Some CTCs have developed community outreach with childcare/preschool programs.
Many service providers work collaboratively within their local early years service partners on various committees and working groups and reciprocally share information to build knowledge and capacity.
Through partnerships, some communities offer community clinics, where community professionals meet with families and their children (0-6) to offer consultation, teaching, and referrals/connections to other services to support children’s development.
Assessment
Assessments are a key component of the Response to Intervention (RTI) approach. In collaboration with families, service providers will complete evidence-informed assessments that consider the child’s skills, abilities, and functioning across all International Classification of Functioning Disability and Health (ICF) framework components that may be impacting their development, including environmental and personal factors (e.g., age, developmental stage, cultural and linguistic background).
General Considerations
Assessments will meet all professional college practice standards and guidelines, including scope of practice, resource requirements, risk management, privacy, competencies and procedures.
Assessments may use a variety of formal and informal tools and approaches (e.g., dynamic assessment) and should be adapted to the needs of the child and family, with consideration for language needs and cultural norms. Assessment, goal setting, and intervention (including introduction of supports and strategies) may occur within the same interaction, enabling service providers to support children and families to efficiently access Tier 2 or 3 intervention.
Whenever possible, the assessment process should also include the provision of evidence-informed information, home strategies and, as appropriate, modeling and coaching of strategies so families can support their children at home. Different cultural norms mean that some parents/caregivers may not see themselves as key participants in the treatment process; service providers should inquire about expectations and collaborate with families to ensure they understand what they are being asked to do and why it is beneficial.
Strategies may also be provided for other contexts, such as childcare or school settings, when applicable, to be shared via the family or directly with other providers (with consent).
Integrated Assessment Processes
Service providers are expected to share information (with family consent) to avoid duplicating assessments when families transition between services. This includes coordinating with District School Boards, whenever possible.
Local agreements should be in place for children to seamlessly transfer between PSL service delivery partners, including to/from rehabilitation services in the local catchment, as applicable.
- This should enable children to access Tier 2/Tier 3 services following an initial assessment at the most appropriate service location, regardless of where the initial assessment was provided.
Multi-Disciplinary Assessments
Multi-disciplinary assessments are an efficient team approach to assessment that can be used when children have identified needs across more than one discipline and/or a diagnostic assessment would benefit from perspectives from multiple disciplines. For example, a child with social communication and sensory needs may be scheduled for a diagnostic assessment with a developmental pediatrician, occupational therapist, and speech-language pathologist together.
Initial Assessment
Within the context of the service delivery pathway, the Initial Assessment (IA), completed by a regulated health professional, is an opportunity to assess children’s function and determine the need and potential for further intervention, following the provision of Tier 1/Universal supports.
In the RTI approach, service providers should confirm with families that an assessment is still required before scheduling the IA. This check-in may occur as part of a routine booking process (e.g., by email) so that an additional contact with the family is not required. Once the family confirms that they have ongoing concerns about their child’s development, an IA is scheduled with the family at a convenient time and location. Virtual assessments may be offered as a choice to families to support access.
The IA should build on information gathered through the intake process so families do not have to re-tell their stories (though they should be welcomed to do so if they wish). This may include using information gathered from the About My Child tool if it was completed with the family through the SmartStart Hubs or information from others (with consent), who may have helped to identify that the child has further needs, beyond Tier 1/Universal supports. All subsequent assessments are considered re-assessments and should build upon information from previous assessments.
For families that were not connected through the SmartStart Hub, but who would benefit from a conversation to further explore their concerns and needs related to their child’s development, a connection should be made to the SmartStart Hub as per local agreements and processes.
Given there may be a wait time between the IA and beginning a recommended intervention, the family will be provided with contact information to encourage the family to contact the service provider if needs change to facilitate continued engagement in their service journey.
For PSL Providers:
In PSL, families will only receive one IA though more than one visit may be required to complete the assessment process. Those who transfer between service providers or re-enter the PSL Program will not undergo another IA.
Mandatory outcome measurement tools are completed at IA for children 18 months and older. For children with permanent hearing loss, outcome measures are completed according to the spoken language outcome monitoring protocols. Exceptions for completion include children for whom the sole area of assessment is feeding/swallowing. See January 2014 PSL Program Outcome Measurement Protocol for requirements and Appendix 6- PSL Program Outcome Measurement and Monitoring for an overview of administration for all children.
For the mandatory outcome measurement and monitoring administration schedule, including at re-assessment, see January 2014 PSL Program Outcome Measurement Protocol. For requirements, see PSL Outcome Measurement Guide 2015 and for an overview of administration for all children, see Outcome Measures.
Re-assessment
Re-assessment is used to determine children’s response to the intervention they have received, occurring at the end of the active intervention and/or following a consolidation period.
- Based on the re-assessment, service providers and families collaboratively plan next steps, including determination of the need for further intervention.
- To monitor progress and inform continued clinical decision-making, re-assessment should be completed at minimum every 6 months.
footnote 41 - In some cases, re-assessment may occur during the same visit as the last scheduled intervention visit.
What’s happening in Ontario?
Some providers schedule “quick” assessments based on the needs profile gathered at intake when mild concerns and needs are identified.
In some regions, local agreements between agencies define specific populations served at each agency. These populations are based on needs identified at intake or directly after assessment.
One region described an integrated model where SLPs from a PSL partner agency participate in multi-disciplinary assessments at their local CTC to collaboratively determine the provider to best support identified needs.
Communicating Assessment Results and Assessment Reports
Assessment results will be communicated to the family (and child, when appropriate) by a regulated health professional and documented as per professional college standards. This includes clearly communicating the difficulties/disorders identified (within the scope of practice) using up-to-date terminology when communicating with families either verbally or in writing.
Assessment reports provided to families will:
- Focus on children's strengths and be written in accessible, culturally appropriate language that is easy for families to understand.
- Communicate findings of the assessment, including identifying any difficulties/disorders.
- Provide a summary of the supportive conversation that occurred as part of the assessment process and not contain new information for the family.
Common assessment report processes and templates within the catchment may help improve system efficiencies and consistency for families ( e.g., establishing local guidance regarding length of reports and when reports should be competed, such as at transitions points or when needs change).
Next Steps after the Assessment
If needs and goals are met through the assessment process, families are supported to transition out of services (see Supportive Transitions: Discharge).
If needs and goals are identified through the assessment process, an intervention(s) must be recommended, in consultation with the family.
Intervention
Response to Intervention Approach – Tiered Service Model
Implementing a Response to Intervention (RTI) model will support provincial consistency in offering families a range of services and will provide ongoing opportunities to evaluate the program.
Research has shown that tiered service models applied in schools (for example, in Rehabilitation Services) are highly rated by professionals and families alike. Partnering for Change (P4C),
The PSL and Children’s Rehabilitation Services programs function within a multi-tiered service continuum by supporting early identification and a range of interventions to meet the needs of children and families. Evidence on tiered, RTI approaches for preschool speech and language programs is limited, as much of the available research has been conducted in education settings.
The RTI pyramid has been adapted from various interprofessional tiered service models
Figure 5: Example of a Tiered Intervention Delivery Pyramid
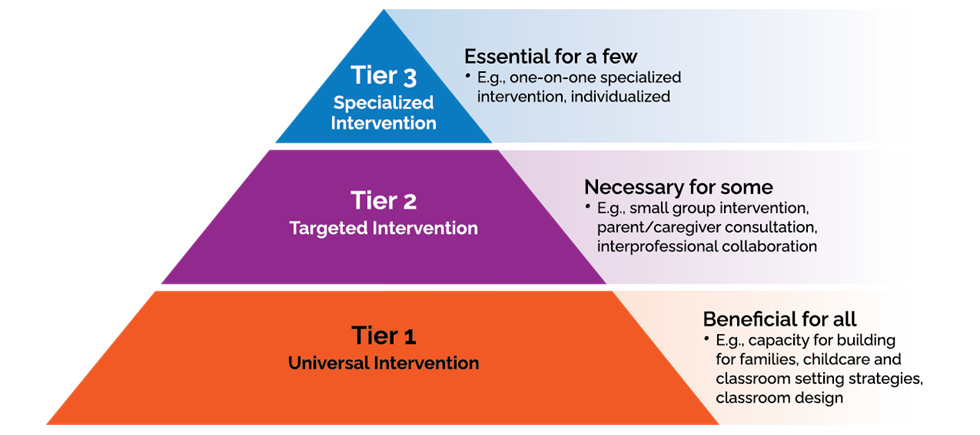
Image of Pyramid from base to top
Tier 1: Universal Intervention. Beneficial for all. E.g., Capacity building for families, childcare and classroom setting strategies, classroom design.
Tier 2: Targeted Intervention. Necessary for some. E.g., Small group intervention, parent/caregiver consultation, interprofessional collaboration.
Tier 3: Specialized Intervention. Essential for a few. E.g., One-on-one specialized intervention, individualized.
Service providers will use clinical reasoning throughout an intervention to adapt and refine goals and intervention approaches based on outcomes and feedback from the family, child/youth, and others, as applicable. Families and other team members will be supported through coaching, training, and check-ins to implement intervention strategies at home and in the community and/or applicable education settings.
Goal Setting
Assessments should provide families (and children and youth as appropriate) with the opportunity to have their questions addressed and discuss strengths and needs to determine goals and next steps. This includes an opportunity to talk about personal and environmental factors that impact their child’s development and family factors that are important for planning next steps, such as transportation needs, cultural relevance, and literacy supports.
In the context of child- and family-centred care, families and service providers will work together to develop functional, strengths-based, and solution-focused goals that are meaningful to children and families. Goals should be specific, measurable, achievable, realistic, and time-limited (SMART).
Connections to Other Supports
Children and their families should also be connected directly to other community services when needs have been identified beyond the scope of the PSL Program or Children’s Rehabilitation Services (e.g., Infant and Child Development Program, Special Services at Home) during an assessment.
Families Stay Connected
Through the RTI approach, service providers are strongly encouraged to check in periodically with families who are waiting for intervention, such as every 3-6 months. This engagement (which can be completed passively, e.g. through automated email) provides an opportunity to stay in touch with the family, address concerns/questions, confirm needs, and re-prioritize services.
At minimum, service providers must provide families with clear information about how to connect with their service provider and be encouraged to follow-up at any time if they have questions, have immediate needs, or no longer require supports. An estimated wait time until the next contact should also be provided so that families know what to expect and when.
What’s happening in Ontario?
Some CTCs stay connected to families to support home practice and consolidation of skills between interventions, so they are not “waiting” between services but rather, receiving ongoing education, coaching, and strategies to be able to continue to support their child at home.
Some regions offer drop-in consultation clinics for families to stay connected and provide home strategies.
Tiered Intervention After Assessment
Assessment will help service providers determine whether children who have been receiving Tier 1/Universal Intervention implemented by family members and/or community and education partners (e.g., general strategies to support following directions) may benefit from more intensive, targeted Tier 2 or Tier 3 Intervention to address specific needs. It should be noted that children may continue to benefit from Tier 1/Universal Intervention while engaging in Tier 2 or 3 Intervention. Children and families may need different levels of support and approaches at different times.
Tier 2 Targeted Intervention
Tier 2 interventions are targeted and are necessary for some who have identified needs that require additional supports beyond Tier 1/Universal intervention.
Tier 2 interventions may include parent training, group intervention, home programming, and collaborative consultation with community partners (e.g., engaging with childcare providers to collaboratively support specific children). A range of interventions should be offered within Tier 2 at different levels of intervention intensity to address a range of needs.
Tier 3 Specialized Intervention
Tier 3 interventions are specialized in that they are essential for a few children who require individualized supports beyond Tier 2 targeted interventions, including addressing urgent needs and children who are at high risk for ongoing difficulties. As with Tier 2 services, families must consent and a health record is required for the child. These interventions may be more intensive and are provided one-on-one in a clinic, educational, or home setting over a specified period.
When more than one service provider is involved in delivering intervention (either within the same discipline or across disciplines), providers will collaborate in a coordinated team approach to meet the needs of the child and family
In alignment with best practices, services required in multiple locations (e.g., home and school) and/or services within the same discipline (e.g., speech needs/goals and language needs/goals) should be supported by the same service provider.
The types of interventions offered within the PSL program are outlined in the PSL HCD-ISCIS Data Tracking Manual, which includes definitions and examples of each intervention type.
Consolidation Period
A consolidation period usually occurs after an active intervention is completed and before another service is provided (re-assessment or intervention). During this time period, the child and parent continue to integrate and generalize information and strategies into everyday activities and remain focused on the same goals that were targeted during the active intervention.
After the consolidation period, a re-assessment may occur if the family has identified further concerns and goals. If the consolidation period extends for a long period of time, a check-in with the family is strongly encouraged.
Clinical Intervention Dosage and Intensity
Along with the type of intervention options identified within each tier as part of clinical service pathways, service provider organizations may choose to provide some guidance to individual service providers regarding intervention intensity, including frequency of services offered (how often) and total number of visits (e.g., up to maximum number of sessions) to manage resources and support consistency.
Families and service providers will work together to make collaborative, evidence-informed decisions to determine the intensity of services provided within the context of their local service system.
Clinical decision making about intervention intensity relies on a multitude of factors and decisions should be made based on the available research evidence for a particular disorder area/need, child and family factors (e.g., child engagement, communication developmental profile, family preferences)
Supportive Transitions
Children and families experience many transitions throughout their lives. Service providers need to consider how natural life transitions (e.g., move to a new home or new service provider) will need to be supported in the service journey within the context of the child and family’s unique experience.
Service transitions can be stressful for everyone. Setting out clear steps, processes and expectations for advance planning and collaboration puts families at the centre of the process, helps to alleviate their anxiety about what happens next, and prepares them for success in the next steps in their service or life journey.
Supportive transition refers to a seamless, streamlined and “warm transfer” of services and supports as children or youth age or their service needs change. This may also include exit from services.
Transition Protocols
PSL Lead Agencies and CTCs will collaborate to develop and implement transition protocols to support the warm transfer of services between service providers using an equitable, integrated wait time management approach. Transition protocols should consider the following, as applicable:
- Expectations for collaboration among organizations (e.g., childcare and/or education partners, the OAP Entry to School program) to provide a supportive “warm transfer” for families in advance of transition:
- Supportive transition refers to a seamless, streamlined and “warm transfer” of services and supports as children or youth age or their service needs change. This may also include exit from services.
- Multiple partners should take a coordinated, team approach to address the holistic needs of the child and family during or in preparation for a transition.
- Processes for consent and information-sharing:
- Between PSL providers, information may include the FOCUS-34 Lifecycle Report and HCD-ISCIS Family Profile.
- Processes for working with families to co-develop a transition plan, including identification of potential issues/concerns in advance of key transition points, as applicable.
- For families accessing Coordinated Service Planning, transitions will be supported in compliance with specific requirements outlined in the Coordinated Service Planning and Policy and Program Guidelines 2017, and in accordance with locally developed formal agreements and/or Memoranda of Understanding (MOUs) with the Coordinating Agency in the catchment.
- Transition planning processes should align with evidence-informed practices as applicable.
footnote 48
Transfers within and between catchments
Transfers within a catchment and between catchments may be between individual service providers or different service provider agencies (e.g., when children transfer from a PSL program to a CTC for SBRS to address ongoing speech-language needs).
In all cases, transfers should honour the original referral date and avoid another IA if one was already completed in the source region, and associated approaches are ongoing.
Depending on circumstances, if sufficient information can be provided to the receiving service provider, children may access an intervention directly (i.e. enter the RTI loop at intervention, rather than at assessment). This practice streamlines service access by building on assessment information, rather than duplicating assessments.
Children identified with permanent hearing loss should be transferred between Infant Hearing Program regions, rather than between PSL Programs to ensure all components of IHP services are transferred, inclusive of SLPs services (e.g., Audiology services, Family Support Worker services, ASL consultation services).
For PSL Providers:
Entry to School services
As with any transfer of services, PSL providers will support a warm transfer by sharing relevant information to Entry to School (ETS) providers (with parent consent) and help prepare the child and family for a service transition. Some children may require collaborative planning to review plans, goals and progress as the child moves between services.
Through the Ontario Autism Program, eligible families are invited to participate in the the ETS program, which helps prepare children who are starting kindergarten or Grade 1 for the first time.
The ETS program includes two main parts. The first part is a six-month, group-based, skill-building program, focused on helping children develop school-readiness skills in six areas: communication, play, social interaction, functional routines, behavioural self-management, and pre-academics, learning, and attention.
For children and families with multiple and/or complex special needs who are receiving Coordinated Service Planning, the Service Planning Coordinator should also be engaged to support coordination of transition planning through a single Coordinated Service Plan.
Given the intensity of service and multi-disciplinary team support provided through the ETS program to meet child and family needs, families may choose to discontinue PSL services while participating in the ETS. In this situation, PSL providers would discharge the child and family from the PSL program once a warm transfer to the ETS providers has been completed.
A child who is registering for and participating in the ETS program may continue to participate in the PSL program if communication needs and goals can be supported through both programs. To avoid duplication in services, providers are expected to coordinate services and align goals to meet the needs of the children and families. For example, the PSL SLP may provide support for implementation of an existing augmentative communication system as the child transitions into the ETS program while all other communication goals and supports are coordinated by the ETS SLP. Once the augmentative communication system has been implemented into the ETS setting, PSL services may not be required and could be discontinued if no further needs have been identified by the family that require support from the PSL SLP. PSL and ETS providers are expected to work together to exchange relevant information, with consent, including the family and child’s needs, goals, and clinical recommendations.
For children enrolled in both programs, the ETS provider will lead the family’s transition to school. As needed, PSL providers may contribute to the transition to school planning, in collaboration with the ETS providers.
Additionally, ETS providers are expected to lead coordination and alignment with the other service providers already working with the child. ETS providers will consult with other clinicians already working with the child, including PSL providers and, if applicable, Coordinated Service Planning providers, to:
- align goals and skill-building with children’s existing treatment plans to avoid duplication, and
- foster shared communication about the child’s strengths and needs to inform the school transition process.
Transitions at School Start
To support seamless, streamlined transitions into school, service providers should operate as a system in the catchment to minimize gaps between programs. Service delivery organizations should make every effort to provide streamlined services so families do not experience entry and exit from multiple programs.
Key considerations for service providers
- PSL Program services are provided until school start at which point children who continue to require services are transitioned to school-based services or community services as needed and informed by the child’s circumstances.
- If families choose to delay school start beyond the earliest date (i.e. kindergarten), PSL services will continue until the child starts school, or until the mandatory school start (Grade 1).
- If the child is participating in the Ontario Autism Program ETS program (which begins six months prior to school start), the program
footnote 49 will lead the transition to school processes even if the child continues to receive services through the PSL Program.
- School-based Rehabilitation Services (SBRS) begins at school start.
- If families choose to delay school start, CBRS occupational therapy and physiotherapy services continue at least until school start and may continue thereafter, depending on local agreements and integration with SBRS; see above for speech language pathology service delivery.
The graphic below depicts the timeline of potential service transitions.
Figure 6: Seamless Transition to School
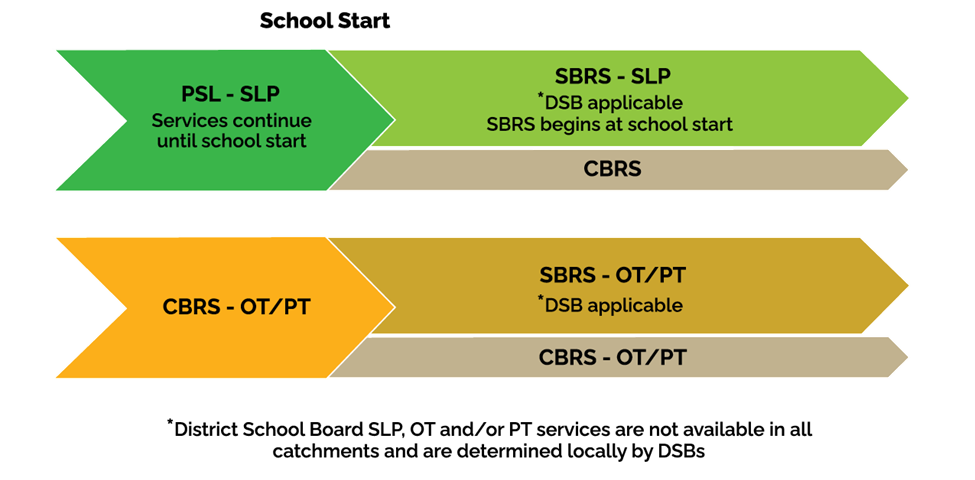
Image contains 2 arrows.
First arrow: PSL – SLP. Services continue until school start.
SBRS – SLP. DSB applicable (District School Board SLP, OT and/or PT services are not available in all catchments and are determined locally by DSBs). SBRS begins at school start. CBRS.
Second arrow: CBRS – OT/PT. School Start. SBRS – OT/PT. DSB applicable. CBRS – OT/PT.
PSL transition plans should be in place for all children who have identified communication needs that will continue to require intervention in school. See HCD-ISCIS PSL Data Tracking Manual for further details.
In general, children who have accessed PSL services and are transferring into SBRS should be considered for triage/prioritization along with other new referrals at school start, in a needs-based approach, taking into account school board-led services. This means that some children may need to be prioritized for immediate short-term service at school start (e.g., to address safety strategies or ensure they receive equipment required to attend school).
Note: Families should be advised that if they contact the PSL Program very close to school start, it may not be possible to access services again due to wait times, even if a re-entry process is in place.
Discharge from Services and Re-entry Mechanisms
Families who are leaving services may experience a range of emotions and concerns, and as with any program, service providers should develop warm and supportive processes for children, youth, and families who are being discharged.
A process should be in place and communicated to families to support service continuity if a child needs to re-enter services after discharge (e.g., if new concerns are identified by the family).
In such cases, the existing profile of the child may be re-opened and the child may re-enter the waitlist for services based on their original referral date. This process supports a family to discontinue services when needs are met, knowing they can seamlessly re-enter the service pathway if needs arise in future. For example, if a child was discharged having achieved appropriate outcomes and then the family re-enters with their child a number of months later, the family will receive a re-assessment, rather than wait “at the end of the line” for an IA. In this way, the family re-enters the RTI loop of services rather than re-starting the service delivery pathway.
When current needs have been met, future needs may be predicted or anticipated (e.g., new equipment required).
In these cases, processes may be in place to monitor progress and check-in with families over time, rather than discharging from services, given the anticipated need for longer term supports over time.
See the Discharge section of HCD-ISCIS PSL Data Tracking Manual for PSL discharge codes.
Footnotes
- footnote[35] Back to paragraph SmartStart Hubs will take a leadership role to help coordinate access to information and a supportive connection to child development services. See SmartStart Hubs Policy and Practice Guidelines for details.
- footnote[36] Back to paragraph Law, J., Reilly, S., & Snow, P. C. (2013). Child speech, language and communication need re-examined in a public health context: A new direction for the speech and language therapy profession. International Journal of Language & Communication Disorders, 48(5), 486–496.https://doi.org/10.1111/1460-6984.12027
- footnote[37] Back to paragraph See SmartStart Hubs Policy and Program Guidelines for expectations on Hubs provision of Family-Based Supports, including F-words for Child Development and Partners 4 Planning.
- footnote[38] Back to paragraph Anaby DR, Campbell WN, Missiuna C, Shaw SR, Bennett S, Khan S, Tremblay S, Kalubi-Lukusa JC, Camden C; GOLDs (Group for Optimizing Leadership and Delivering Services). (2019). Recommended practices to organize and deliver school-based services for children with disabilities: A scoping review. Child: Care, Health and Development, 45(1), 15-27. https://doi.org/10.1111/cch.12621
- footnote[39] Back to paragraph Missiuna, C., Pollack,N., Campbell, W., DeCola, C., Hecimovich,C., Sahagian Whalen, S., Siemon, J., Song, K., Gaines, R., Bennett, S., McCauley, D., Stewart, D., Cairney, J., Dix, L., & Camden, C. (2017). Using an innovative model of service delivery to identify children who are struggling in school. British Journal of Occupational Therapy, 80(3), 145-154. "https://doi.org/10.1177/0308022616679852
- footnote[40] Back to paragraph Westby, C., & Washington, K. N. (2017). Using the international classification of functioning, disability and health in assessment and intervention of school-aged children with language impairments. Language, Speech, and Hearing Services in Schools, 48(3), 137–152. https://doi.org/10.1044/2017_LSHSS-16-0037
- footnote[41] Back to paragraph This is an expectation identified in the PSL Program Outcome Measurement Protocol and PSL HCD-ISCIS Data Tracking Manual.
- footnote[42] Back to paragraph Missiuna, C. A., Pollock, N. A., Levac, D. E., Campbell, W. N., Whalen, S. D. S., Bennett, S. M., Hecimovich, C. A., Gaines, B. R., Cairney, J., & Russell, D. J. (2012). Partnering for Change: An innovative school-based occupational therapy service delivery model for children with developmental coordination disorder. Canadian Journal of Occupational Therapy, 79(1), 41-50. https://doi.org/10.2182/cjot.2012.79.1.6
- footnote[43] Back to paragraph CanChild Centre for Childhood Disability Research. (2014). An Evidence-Based Collaborative Framework for Integrated School-Based Rehabilitation Services.
- footnote[44] Back to paragraph Ontario Ministry of Education. (2013). Learning for All: A Guide to Effective Assessment and Instruction for All Students, Kindergarten to Grade 12.
- footnote[45] Back to paragraph Bexelius, A., Brogren Carlber, E., & Löwing, K. (2018). Quality of goal setting in pediatric rehabilitation- a SMART approach. Child: Care, Health and Development, 44(6), 850-856. https://doi.org/10.1111/cch.12609
- footnote[30] Back to paragraph Hao, Y., Franco, J. H., Sundarrajan, M., & Chen, Y. (2021). A pilot study comparing tele-therapy and in-person therapy: Perspectives from parent-mediated intervention for children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 51(1), 129–143. https://doi.org/10.1007/s10803-020-04439-x
- footnote[46] Back to paragraph This may include service providers from District School Boards or delivering the Infant & Child Development Program or Ontario Autism Program.
- footnote[47] Back to paragraph Zeng, B., Law, J., & Lindsay, G. (2012). Characterizing optimal intervention intensity: The relationship between dosage and effect size in interventions for children with developmental speech and language difficulties. International Journal of Speech-Language Pathology, 14(5), 471–477. https://www.tandfonline.com/doi/full/10.3109/17549507.2012.720281
- footnote[48] Back to paragraph Canadian Association of Paediatric Health Centres (2016). A Guideline for Transition from Paediatric to Adult Health Care for Youth with Special Health Care Needs: A National Approach.
- footnote[49] Back to paragraph See separate OAP requirements.